Thursday, August 31, 2023
< + > Can wireless diagnostic tools transform chronic care management?
< + > HFMA Edition: How Are You Incorporating AI and Technology like ChatGPT Into Your Organization or Product?
The overarching goal of incorporating AI into the world of healthcare has always been to make the lives of our practitioners and patients easier. Sometimes this can mean using chatbots so patients can have an immediate response to their questions. Sometimes this can mean letting an AI run through the mundane repetitive tasks of the practitioners, freeing up their schedules for what really matters. There are just so many areas of healthcare that the possibilities of how and where you integrate new technology like AI and ChatGPT into your organization are endless. To prove this point we reached out to three different organizations at the HFMA annual conference to hear their thoughts on how they’re looking to incorporate AI and we got back three very different answers.
Laxmi Patel, Chief Strategy Officer at Savista said “One of the things we’re looking at at Savista is related to data analysis and integration of those trends into our outcomes. One of the examples is coding automation, so analyzing large sets of data from an accuracy and an efficiency standpoint and tying it to financial outcomes.”
“What AI helps us do is review every patient chart, so then we have the ability to give our clients the best solution for their teams. It helps them operate at the top of their license as well as work on an exception basis, so they’re spending their valuable time on the hardest cases and we can take care of the ones that are less complex,” said Ruth Nacey, Director of Product at SmarterDx.
Jason Considine, Chief Commercial Officer at Experian Health said “We’ve been able to predict over 50% of the claims that are going to get denied in our customer’s claim flow processes and by implementing those technologies we’ve seen them reduce their claim denials by 5%.”
Watch the video below to hear their full answers!
If you liked this video, be sure to subscribe to Healthcare IT Today on YouTube to be notified of our latest videos.
Huge thank you to everyone who took the time out of their day to come speak with us to make this video possible! And thank you to all of you for taking the time out of your day to read this and watch the video!! We wouldn’t be here without your support and we would love to hear from you as well. Comment down below or on social media on where you think AI and technologies like ChatGPT should be incorporated into the world of healthcare!
< + > Social Isolation: A Broader View
The previous articles in this series explain how technology is being used to bring people out of social isolation. But sometimes, loneliness springs from other mental conditions, such as anxiety and depression. Targeting these problems can help bring the patient back into a community.
Treating Psychological Conditions
One of subtler negative effects of moving online is that people lose the small, casual social interactions that previously would buoy their spirits and leave them smiling: asking for help from the post office staff, chatting with cashiers while bagging purchases, greeting people in the elevator, etc. The millions of people working from home during the COVID-19 shutdown—and many are still doing so—lost the multi-layered connections they had with their fellow workers, and have found that they can’t reforge such bonds online.
Ideally, we’d all find ways to replenish these weak social ties. But given the centrifugal pull in modern society, some companies are using computers to provide social interaction. Recent big advances in AI, chat, and voice synthesis make it possible to shape personalized conversations and simulate human contact. Some people may find that trrend manipulative or creepy, but such computerized interactions have been shown to combat loneliness.
I spoke with Dor Skuler, CEO and cofounder of Intuition Robotics, about their ElliQ companion for the elderly. It asks questions to determine their needs and then carries on the kinds of sympathetic dialogs that a family member or friend would offer (Figure 1). ElliQ can check on users’ health and suggest positive steps to take. Some of these steps can reduce social isolation, such as encouraging the user to take a photo and send it to a family member.

Skeptical? Intuition Robotics finds that ElliQ users have seen an 80% reduction in their perception of loneliness. Users average more than 30 interactions per day, and increase their use if they stay with the service for more than 30 days. Being a learning system, ElliQ gets better as the user stays with it.
Since 2022, many states and aging agencies have offered ElliQ for free because it helps people age at home. Other users pay a subscription. Because ElliQ is funded by these payments, Intuition Robotics doesn’t have to ” monetize people” by marketing a product or selling data. Thus, the service can focus on providing exactly what each user needs.
Like other institutions, health care providers have installed chatbots to handle a high volume of requests from clients. The chatbots can’t provide the same subtlety as a trained human, but can spread a service’s resources further and potentially reach more people.
Matt Hollingsworth, CEO of Carta Healthcare, talked to me about the potential of the metaverse: online spaces where people can interact with a lot of visual and auditory stimulation. Although projects by Meta and other companies haven’t lived up to the promise of the metaverse (which goes back a couple decades with Second Life), Hollingsworth says that Gather has found some success at building person-to-person connections.
Sandeep Shah, founder and CEO of Skyscape, says their Buzz service already uses AI to turn up risks while it facilitates patient interactions with clinical and family care givers. Shah expects sentiment analysis to be part of future services that handle patient communications.
Humane Technology in a Less Humane World
Our epidemic of loneliness has crept up on us as the things that humans used to do naturally are being digitized. It’s hard even to drag your doctor away from the computer to talk to you.
Susan Smith, a nurse who is a clinical content analyst at Sagility, says many people don’t notice that they’re socially isolated and don’t attribute their feelings of depression, anxiety, or difficulty coping to social isolation. Teun Schutte, managing consultant of digital strategy in healthcare at Mobiquity, said that young people in particular don’t make the connection between mental illness and social isolation. Education is needed about the importance of connections.
Technology, as this series has shown, can be used to strengthen social connections as well as to weaken them. By making us more conscious of our need for other people, the technologies might push us to head down to the park or basketball court and interact with somebody.
< + > Revolutionizing Fertility Care: Femtech CEO Weighs in on the Power of Remote Monitoring and Advancing Technologies
The following is a guest article by Sylvia Kang, Co-Founder and CEO at Mira
In recent years, the landscape of reproductive health has witnessed a significant shift with technological advancements toward fertility care. As the CEO of a leading Femtech company, I have witnessed firsthand the transformative potential of at-home remote monitoring and innovative technologies in empowering individuals and couples on their reproductive journey. Let’s explore the benefits of embracing remote monitoring in fertility care—and the broader impact of advancing technologies, such as AI, in shaping the future of reproductive health.
The Rise of At-Home Health Solutions: A Paradigm Shift
The global pandemic catalyzed the home health sector, driving investments in remote healthcare solutions to unprecedented levels. According to a report by 7WireVentures, investments in at-home health companies soared from $2.2 billion in 2020 to $4.7 billion in 2021. The pandemic-induced necessity for social distancing and limited access to healthcare facilities led to a 29% increase in remote healthcare services among U.S. adults. A McKinsey & Company article revealed that telehealth usage witnessed a staggering 38x surge compared to pre-pandemic levels, and 60% of consumers expressed interest in a broader set of virtual health solutions. This shift mirrors the medical community, with 58% of providers viewing telehealth more favorably and 84% of physicians offering virtual visits.
The Power of At-Home Remote Monitoring in Fertility Care
Traditional fertility care has limitations, often requiring frequent clinic visits for blood sampling to measure hormone levels. The COVID-19 pandemic exposed the inefficiencies of this approach, prompting a reevaluation of how technology could bridge the gap between doctors and patients remotely. Innovative technologies, particularly AI, have emerged as key enablers of better patient experiences. It also enables broader access to fertility care. AI can enhance fertility treatment success rates, lower medical expenses, and offer greater transparency throughout the in vitro fertilization (IVF) process.
These are some of the many reasons why I created Mira. The Mira Analyzer allows for quantitative hormone measurements in urine. It’s an at-home, remote, AI-driven monitoring solution that replaces traditional blood sampling, offering a more convenient and pain-free alternative. Individuals can monitor their hormone levels from the comfort of their homes—reducing the need for frequent clinic visits and minimizing testing costs. Users feel more empowered by knowing what is going on in their bodies. They also can partner with their medical team to share accurate, real-time information about their hormones.
Looking Towards the Future of Fertility Care
The integration of at-home remote monitoring and the collaboration between fertility tech and clinics hold promising implications for the future of reproductive health. As we embrace technological advancements, we empower patients with a greater understanding of their fertility status. Remote monitoring streamlines the process and fosters a deeper connection between doctors and patients.
Moreover, the use of AI in fertility care heralds a new era of personalized treatments. By analyzing vast data, AI algorithms can offer tailored insights into the best course of action for individual patients, increasing the chances of successful fertility treatments. This level of personalization brings hope to those who have faced challenges in their reproductive journey—offering them renewed possibilities.
Empowering Reproductive Health Through Technology
In conclusion, fertility care is on the cusp of a revolutionary transformation, and embracing at-home remote monitoring and advancing technologies are keys to unlocking its full potential. As a thought leader in the Femtech industry, I believe these innovations will continue to improve patient experiences, reduce barriers to care, and empower individuals and couples as they navigate the intricacies of their reproductive health.
By championing the adoption of remote monitoring and fostering collaboration between fertility tech and clinics, we can create a future where fertility care is more accessible, personalized, and successful. The advancements in AI technology offer hope for patients: and the synergy between human expertise and cutting-edge algorithms promises to redefine the possibilities of reproductive health.
As we progress, the medical community, policymakers, and individuals should embrace these advancements and work together toward a brighter future for fertility care. With the power of remote monitoring and advancing technologies at our fingertips, we can unlock the doors to new beginnings and transform the landscape of reproductive health for generations to come.
 About Sylvia Kang
About Sylvia Kang
Sylvia Kang is the Co-Founder and CEO of the health tech company Mira. She holds an MBA from Cornell University, and a MS in Biomedical Engineering from Columbia. Before she started Mira, she was in business director roles in a Fortune 500 life science company, running a $100M global business. Sylvia is also a Concert Pianist. She has won multiple international piano competitions in France, China, and Hong Kong.
< + > Preventative Health and Longevity Company, Viome Life Sciences, Closes $86.5M Oversubscribed Series C Funding Round
Additional Financing Supports the Further Development of its Suite of Advanced Personalized Health Tests and Expansion into Key Nationwide Retailers such as CVS
Viome Life Sciences, a longevity company committed to translating scientific advancements into practical and individualized health solutions, today announced the successful closure of its $86.5 million oversubscribed Series C funding round. Lead investors include Khosla Ventures and Bold Capital with participation from other existing ones as well as new ones. The raise brings Viome’s total to $175 million and will be used to support research and development and retail expansion efforts.
Today also marks the launch of Viome’s groundbreaking Gut Intelligence Test into 200 CVS locations nationwide. It will be the first-ever gut test available in the national retail chain both online and in-store, underscoring the test’s strong consumer demand and the need for health optimization tools. This news comes on the heels of Viome’s Oral Health Solutions announcement last month which applied its holistic approach and proprietary RNA sequencing technology to usher in a new era of oral health with an emphasis on prevention and long-term care.
“In a world where healthcare has often been reactive, treating symptoms and targeting diseases only after they manifest, Viome is pioneering a transformative shift by harnessing the innate power of food and nutrition. Our mission is not just to prolong life but to enrich it, enabling everyone to thrive in health and vitality,” said Viome Founder & CEO, Naveen Jain. “At Viome, we’re empowering our customers with an individualized nutrition strategy, cutting through the noise of temporary trends and one-size-fits-all advice. We’re on a journey to redefine aging itself, and we’re invigorated by the support of our investors and customers. Together, we’re building pathways to wellness that hold the potential to enhance the lives of billions of fellow humans across the globe.”
Viome’s unique perspective on health goes against a one-size-fits-all diet and uses science to compute the optimal outcome for each consumer based on their unique human and microbial gene expressions. Today’s nutritional practices do not account for each person’s biochemical individuality and are contributing to the onset and progression of many chronic diseases. Viome’s data-driven approach is highly individualized and doesn’t rely on generic nutritional guidelines that treat all humans as similar. Utilizing AI and advanced algorithms to analyze the world’s largest gene expression data from over 600,000 samples, Viome has developed at-home tests and custom-made health products to provide each individual with the precise nutrition their body needs. This includes a supplement formula made unique to every single individual as well as a personalized biotic blend for gut health and personalized oral biotic lozenges, for oral microbiome health.
“We invested in Viome because of its unique RNA technology and cutting-edge AI which when combined with its massive bank of biological data has the potential to prevent an epidemic of chronic diseases like mental health, metabolic health, cognitive health, and digestive health,” said Robbie Schwietzer, Partner at Khosla Ventures.
Viome was founded in 2016 and is backed by a team of world-class industry experts, translational scientists, nutritionists, researchers, doctors, and advisors focused on a single mission: to improve health by delivering scientific breakthroughs that address the root causes of chronic diseases, cancer, and aging. Viome believes that by further understanding the way the microbiome interacts uniquely with every individual, it can empower individuals with insights and actionable recommendations that are needed to live a long and healthy life.
The Series C funding round represents a significant milestone for Viome, showcasing its position as a leader in science-backed, personalized health solutions. For more information about Viome and its solutions, please visit viome.com.
About Viome
Viome is a pioneering longevity and preventative healthcare company committed to bridging the gap between scientific breakthroughs and their practical implementation as health solutions. Utilizing cutting-edge AI and the world’s largest gene expression database, Viome’s home-based tests offer individuals personalized nutritional guidance and innovative microbiome health products to enhance both lifespan and healthspan.
Viome has empowered over half a million users with its unique approach that marries groundbreaking proprietary RNA sequencing methods with AI technology. This combination analyzes epigenetic biomarkers, providing robust, AI-driven health insights that contribute significantly to promoting a healthy lifespan.
Together with its top-tier precision nutrition recommendations, Viome offers a comprehensive and personalized solution to aging – at its optimum. This is more than just health optimization, it’s a revolution in understanding how we age and enabling us to do so with vitality and wellness.
Originally announced August 18th, 2023
Wednesday, August 30, 2023
< + > Interoperability roundup: EHI compliance guidance, LOINC updates and more
< + > Dr. Temi, The Autonomous Robot Will See You Now
It seems we’re just at the start of robots in healthcare. We see them moving around supplies. We see robots working in the pharmacy. Plus, we have a long list of robots doing virtual tasks. When I came across the Dr. Temi robot, it was the first application of an autonomous robot to assist nurses and doctors that I’d seen.
At the HIMSS annual conference, we sat down with Yaron Yoels, CMO at Temi Robot, to learn more about Dr. Temi, an autonomous robot for patient care. What’s cool about this robot is that it doesn’t need a nurse to get to the bedside. The robot can go to the room requested by the doctor autonomously where they can do a telemedicine visit with the patient using the doctor’s cell phone or computer.
While Dr. Temi has a high resolution camera for telemedicine and things like wound care, it also comes built in with a blood pressure cuff, pulse oximeter, 5 lead ekg, digital stethoscope, and can do continuous temperature. All of these devices are connected to the robot which can communicate the findings remotely to the doctor or nurse that needs the information or on the robot’s screen.
Another cool feature of Dr. Temi is that it can follow the doctor or nurse autonomously as the doctor or nurse walks around. The Temo Robot is being used in hospitals, nursing homes, and home care. Check out the demo of Dr. Temi to see it in action and to learn more.
Learn more about Temi: https://www.robotemi.com/
Listen and subscribe to the Healthcare IT Today Interviews Podcast to hear all the latest insights from experts in healthcare IT.
And for an exclusive look at our top stories, subscribe to our newsletter.
Tell us what you think. Contact us here or on Twitter at @hcitoday. And if you’re interested in advertising with us, check out our various advertising packages and request our Media Kit.
< + > How Technology Can Overcome Social Isolation
The previous article in introduced the topic of social isolation and showed its relationship to the subjective feeling of loneliness. Now we’ll start to look at the use of technology (which has been implicated in making these conditions worse) to try to improve them.
Physically Connecting Lonely Individuals
mPulse Mobile evaluates patient needs and suggests local resources they can tap, including peer groups. The service gets data from patient records through AI and natural language processing (NLP). as well as from what the patient says to the service. According to Eden Brownell, director of behavioral science, mPulse Mobile is always listening for a potential mental health concern or an indication that the patient is isolated.
In addition to sending the patient automated messages, the service can bump the patient up to a care manager or nurse to handle an important health matter.
Another service that helps connect patients to their friends and family (as well as clinical caregivers) is PointClickCare. It serves more than 27,000 long‐term and post‐acute care providers, more than 3,100 hospitals and health systems, and 2,200 ambulatory clinics, along with more than 70 state and federal government agencies.
Sagility also uses care managers and online tools to help improve social connections, this time focusing on helping the elderly stay in their homes. A big focus of their Aging in Place service is helping keep the patients engaged with caregivers and families. Susan Smith, a clinical content analyst at Sagility, says they try to educate their clients to find resources for themselves.
James Maskell, founder of HealCommunity, says that online services have some advantages over in-person clinics: They’re always available and can be used without transportation.
Providing Online Connections
As we’ve seen, many people don’t feel safe with the people around them. When I talked to services that form communities, the term “safe space” came up routinely as a contrast to the rejection or abuse that people suffer from in their own communities and on social media.
College students can use Peer Community, a service of TimelyCare, to form supportive communities online. TimelyCare provides licensed clinical staff, supported by AI, to monitor forums and prevent abuse. To further protect students, all posts are anonymous.
TimelyCare has found that the most common reason students use the service is to form relationships. Anxiety and depression are common reasons as well.
Offered at more than 300 U.S. colleges and universities, TimelyCare currently serves more than two million students. A student is authenticated by signing in through the email address and password they use for access to other campus services.
If a posting indicates that the student needs more help than an anonymous forum can provide, a care coordinator is notified and will reach out to the student. However, half of the students who have used Peer Community have not visited a health care provider since they came to campus.
Teun Schutte, managing consultant of digital strategy in healthcare at Mobiquity, says that online connections are useful for patient communities. Many people with a disease are isolated and don’t know anyone else with the disease. Along those lines, one couldn’t cover online support groups without mentioning PatientsLikeMe, which has now served more than 850,000 patients.
In addition to perusing PatientsLikeMe’s extensive library of symptom reports, medication reports, symptom reports, and patient-reported outcome measures (PROs), the patients form support groups so that they “don’t feel like they are alone,” according to Dr. Kate Burke, senior medical advisor at PatientsLikeMe. Groups also have trained moderators.
IT consulting company Avanade provides another platform for coordination and relationship building. According to Christiana Voelker, healthcare industry lead at Avanade, their tools can help build patient communities and support care in the home. For instance, Avanade’s Consumer Outreach uses Microsoft Dynamics Marketing to connect patients with caregivers and personalize communications.
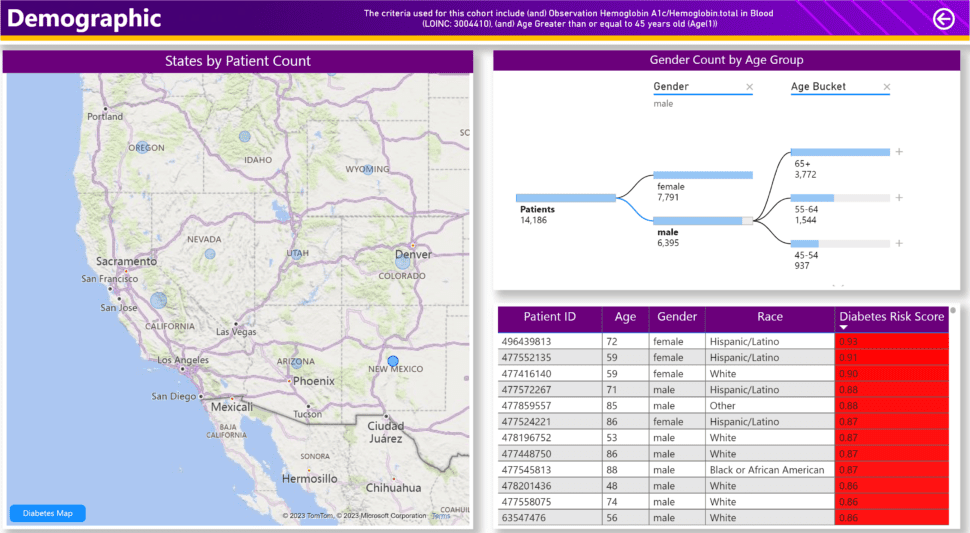
The company’s cohort browser (Figure 1) searches patient data to find people who might be appropriate for a peer group: for instance, people of a certain age with high A1C. A clinician can run the cohort browser and then invite a patient into a group, such as a childbirth class or diabetes support. In addition to support groups, Avanade’s platform can support virtual family visits, as well as connect people for fun, such as a cooking class.
Anyone who has participated in group music making, particularly where singing is involved, knows what a powerful bonding experience it is. According to Andy Tubman, co-founder and chief clinical officer at SingFit, singing in particular promotes social bonding by releasing oxytocin in the singers.
Although most SingFit activities are done in person, it offers some online services. Machine learning is employed to set up playlists for singing as a cognitive exercise. One SingFit app allows a caregiver to input information about a patient and get an appropriate playlist. Another service, offered in some hospices, allows music therapists to guide people to sing through video.
The final article in this series will look at the use of technology to treat mental health conditions that contribute to loneliness.
Tuesday, August 29, 2023
< + > Tackling healthcare AI's bias, regulatory and inventorship challenges
< + > Streamlining Workflows Increases Access for Children with Autism
There are not enough licensed behavior analysts to help children in the US diagnosed with autism spectrum disorder (ASD). To improve access, CentralReach is using technology to simplify, automate, and streamline the many manual tasks related to Applied Behavior Analysis (ABA) – a key therapy that helps people with autism learn helpful behaviors.
Healthcare IT Today had the opportunity to sit down with Chris Sullens, Chief Executive Officer and Nissa Van Etten, Director of Assessment & Clinical Training at CentralReach to find out more about their solution and about the current state of autism services in the US.
Insufficient Care for Autism
In 2023, the CDC reported that approximately 1 in 36 in the US have been identified with ASD. This means that there are roughly 2M children under the age of 18 who are on the autistic spectrum.
According to experts, early intervention affords the best opportunity to support health development and helps people with ASD throughout their life. Applied Behavior Analysis (ABA) is an evidence-based treatment that is widely accepted as the best way to treat autism spectrum disorders.
With only 57,000 board-certified behavior analysts and just over 33,600 ABA therapists in the US, access to ABA therapy is challenging.
CentralReach recognized this gap and has a built an ABA practice management and data collection platform to help streamline the numerous manual administrative tasks.
Streamlining Workflows Leads to Improved Access
“One of the things we have done here at CentralReach is to streamline the assessment process,” explained Van Etten. “We offer CR assessments which combine ABLLS-R and AFLS assessments. By combining these two, we allow clinicians to do early intervention while at the same time help build towards the skills needed for adulthood.”
Assessments of Basic Language and Learning Skills, Revised (ABBLS-R) allow ABAs to identify deficiencies in language, academic, self-help, and motor skills and then implement individualized interventions. Assessment of Functional Living Skills (AFLS) is a way to evaluate and teach functional self-help skills so those with autism can become more independent.
“With all the data now stored in the database, it can easily be recalled,” said Sullens. “I can quickly see what the assessment looked like at intake, then every six months after. That allows them to quickly see progress over time which can be very insightful. Of course, with all that data, we can also do a lot more analysis and reporting that would not be possible with manual tracking.”
According to Sullens and Van Etten, organizations that have implemented CentralReach have seen a noticeable improvement to their workflow. Staff are spending less time on paperwork and have more time for patients as well as more capacity to take on new patients. In this way, CentralReach is helping to improve access to care for children with ASD.
Watch the interview with Chris Sullens and Nissa Van Etten to learn:
- More about the current state of autism care in the US
- How CR Assessments work in CentralReach
- What enhancements are on being added over the next 12 months
Learn more about CentralReach at https://centralreach.com/
Listen and subscribe to the Healthcare IT Today Interviews Podcast to hear all the latest insights from experts in healthcare IT.
And for an exclusive look at our top stories, subscribe to our newsletter.
Tell us what you think. Contact us here or on Twitter at @hcitoday. And if you’re interested in advertising with us, check out our various advertising packages and request our Media Kit.
< + > HCA working with Google Cloud on clinical generative AI
< + > The Lonely Epidemic: Social Isolation and Technology
Alarming effects have been found from recent digital technologies on social connections and mental health. The Surgeon General issued a highly publicized advisory on loneliness and another on youth, both replete with evidence of the harm done by social media and the internet generally. But can digital technology also improve social connections?
While the harm done by digital media to many people has been well demonstrated, there are also people who thrive on digital connections, particularly people from marginalized groups who have trouble finding each other in physical settings). The Surgeon General advisory on youth points that out on page 6.
Another at-risk population is the elderly. The National Academy of Sciences finds that 43% of adults over the age of 60 report feeling lonely. Clinicians and payers would also be interested in the study’s finding that this loneliness makes it harder for these people to use the health care system. It’s natural to lose social contacts as you get older: your friends and family are moving away or dying, you find yourself unable to drive and get around, and you may have to leave your home and familiar friends for an institutional setting.
Making Social Media More Social
Sara Shanti, a partner specializing in health care at law firm Sheppard Mullin, says that social media and technology platforms could be engineered to do better at forming healthy communities and positive interactions.
When conversation turns to depressing or difficult topics, the platform could prompt members to deal with the feelings more constructively. For instance, it could ask a young person to describe a difficult time in their life and how they got through it, or discuss their plans for the future.
Gamification is a powerful tool for behavior change. A conference called Games for Health brought together practitioners for several years.
Shanti and Dr. Wen Dombrowski, chief convergence officer of CATALAIZE, point out that social networking platforms can bring together people with shared interests such as music, arts, health conditions, and social causes. Some sites are general platforms that engage people with many different interests, while others are designed specifically for a particular niche.
Shanti also sees technology that helps people find peers in their local community and encouraging them to meet at a gym, gardening club, etc. Religious institutions, which are well-known for forming strong communities, could also be found online.
Shanti says the institutions with the incentives to improve the use of technology to solve isolation include payers and employers, especially employers with remote workers.
Many Ways to Approach Loneliness
As pointed out by Dor Skuler, CEO and cofounder of Intuition Robotics, loneliness is not the same as social isolation. Loneliness is a subjective feeling, which is often caused by social isolation but can also spring from a feeling of alienation.
Thus, individuals who are different from others in some way—because of race, disability, or sexual preference—often feel lonely even when they’re surrounded by people. Not only do the people surrounding the marginalized person fail to provide emotional support; they may even be threatening. Furthermore, someone is who is depressed can feel alienated from other people, with a similar sense that they are a threat.
Thus, approaches to social isolation include the following interventions, all of which we’ll see in this series:
- Physically connecting the lonely individual with others in their geographic community
- Providing online connections to people who can’t meet other people face-to-face for health, logistical, or other reasons
- Treating the underlying psychological depression and sense of alienation
How do clinicians and public health officials measure loneliness, given how subjective it is? Skuler says that the current standard is the UCLA Loneliness Scale. Other universities are working on sales that do better at measuring objective conditions of loneliness and social isolation. Surveys rely on patient-reported outcome measures (PROs) to indicate isolation and loneliness.
Upcoming articles in this series will look at each of the three types of interventions listed here.
< + > Strengthening Email Cybersecurity for Health Practices: Safeguarding Sensitive Patient Data
 The following is a guest article by Oliver Patterson, Director of Product Management, VIPRE Security Group
The following is a guest article by Oliver Patterson, Director of Product Management, VIPRE Security Group
In the digital era, email has become an indispensable communication tool for healthcare organizations. However, it also poses significant cybersecurity challenges, as sensitive patient information is vulnerable to breaches and phishing attacks. As the sector continues to evolve, we’ve got to continue exploring and understanding the importance of email security for health practices — and how advanced email security solutions can address these challenges effectively.
Understanding Email Cybersecurity Challenges in Health Practices
Health practices face unique cybersecurity challenges because of the sensitive nature of the patient information they collect and house. According to various studies, the healthcare industry experiences a high frequency of data breaches and cyberattacks.
According to the IBM “Cost of a data breach 2022” report, the cost of a breach in the healthcare industry went up 42% since 2020. For the 12th year in a row, healthcare had the highest average data breach cost of any industry. The average cost of a healthcare data breach in 2022 jumped $1 million to a record high of $10.1 million, which is 9.4% more than in 2021 and 41.6% more than in 2020.
Phishing, for example, is one of the most common cyber threats in the economy — 81% of organizations affected by phishing in 2022. Healthcare is no exception. Phishing attacks are one of the most common attacks in the sector. Phishing can range from mass email campaigns designed to trick employees into giving up passwords, to highly targeted campaigns designed to illicit fake invoice payments.
Likewise, a subset of phishing is business email compromise (BEC). Here, attackers try to breach email accounts to send out even more realistic phishing scams. Known as the “26-billion-dollar scam” by the FBI, BEC attacks can be highly effective in the healthcare environment. Healthcare organizations will spend $125 billion USD on cybersecurity from 2020 to 2025.
Email-related cybercrime, including phishing attacks and business email compromise, in the healthcare industry rose by 42% last year.
Features and Benefits of an Advanced Email Security Solution
To combat these challenges, advanced email security solutions offer a range of features designed to enhance protection and minimize risks. These solutions provide robust email filtering and attachment scanning capabilities, leveraging technologies like machine learning and artificial intelligence to identify and block malicious content effectively.
Advanced anti-phishing and URL protection features also help detect and prevent phishing attempts, safeguarding healthcare organizations from falling victim to fraudulent schemes. Data loss prevention (DLP) capabilities play a vital role in ensuring compliance by identifying and protecting sensitive patient data within emails. For example, users are notified to correct their actions before hitting the send button, reducing the time spent by IT and other departments who would otherwise need to investigate these preventable incidents. Likewise, data loss awareness tools help organizations reduce data leakage through misaddressed emails.
In this instance, healthcare’s email security challenges are enhanced through encryption and secure communication features, like adding add an extra layer of protection, preventing unauthorized access to confidential information. Additionally, user awareness and education initiatives raise the overall cybersecurity posture of health practices, so educating employees about email security best practices is an excellent starting point.
Mitigating Vulnerability and Enhancing Protection
An advanced email security solution significantly mitigates vulnerabilities in health practices. By effectively blocking malicious emails and attachments, it reduces the risk of malware infections and data breaches.
According to the “2021 Data Breach Investigations Report” by Verizon, 85% of all breaches involve human interaction, often through email phishing attacks. In healthcare, “basic human error continues to beset this industry as it has for the past several years. The most common error continues to be misdelivery (36 percent), whether electronic or paper documents.”
Advanced solutions equipped with real-time threat intelligence can identify and neutralize emerging threats promptly, ensuring healthcare organizations stay ahead of cybercriminals. These solutions also aid in enforcing compliance with regulatory standards such as the Health Insurance Portability and Accountability Act (HIPAA), minimizing the risk of penalties and legal consequences for non-compliance.
Seamless Integration and User-Friendly Experience
Implementing an advanced email security solution offers seamless integration with existing email systems and platforms, facilitating a smooth transition without causing significant disruptions to daily operations. In addition, these solutions are specifically designed to streamline the deployment and configuration process, ensuring a hassle-free implementation experience for healthcare organizations.
One of the key advantages of advanced email security solutions is their user-friendly interfaces and simplified administration. As a result, Healthcare IT teams can easily navigate and manage email security solutions. In addition, the intuitive interface allows for efficient configuration, monitoring, and management of email security settings, ensuring optimal protection without placing an excessive burden on IT staff.
Automated updates and continuous threat intelligence are fundamental aspects of advanced email security solutions. These solutions regularly receive updates and patches that address emerging threats, vulnerabilities, and security enhancements. This proactive approach ensures the solution remains up-to-date with the latest security measures, protecting healthcare organizations against evolving and sophisticated email-based threats.
Continuous threat intelligence is another crucial aspect of advanced email security solutions. By leveraging threat intelligence feeds and real-time analysis, these solutions can identify and block new and emerging threats in a timely manner. This proactive defense approach allows healthcare organizations to stay ahead of cybercriminals, reducing the risk of successful email-based attacks.
Moreover, advanced email security solutions often provide centralized management consoles, allowing IT administrators to monitor and enforce security policies across the organization efficiently. This centralized approach ensures consistency and compliance with security protocols and regulations, simplifying managing email security on a larger scale.
In addition to seamless integration and user-friendly administration, these solutions often offer reporting and analytics capabilities. IT teams can access detailed reports and insights into email security events, enabling them to track and assess the effectiveness of the implemented security measures. This information can guide future security enhancements and strengthen the overall email security posture of the healthcare organization.
Overall, implementing an advanced email security solution offers seamless integration with existing systems and provides user-friendly interfaces, simplified administration, automated updates, continuous threat intelligence, and comprehensive reporting capabilities.
These features create a robust and efficient email security environment that safeguards sensitive patient data while minimizing disruption and maximizing protection against evolving email threats.
Conclusion
With the increasing cybersecurity threats faced by health practices, prioritizing email security is paramount. Advanced email security solutions provide a comprehensive approach to protecting sensitive patient data, mitigating vulnerabilities, and ensuring regulatory compliance.
By leveraging features such as robust filtering, anti-phishing measures, data loss prevention, encryption, and user education, healthcare organizations can enhance their email security posture and safeguard patient information effectively.
< + > ChatGPT scored 72% in clinical decision accuracy, MGB study shows
< + > Royal Flying Doctor Service moves to cloud for EMR management
Monday, August 28, 2023
< + > Upcoming Healthcare Regulations and Their Impact on Healthcare IT
For something as important and as sensitive as healthcare, there are plenty of rules and regulations in place to protect both patients and organizations. However, with healthcare being ever-evolving our regulations are also ever evolving. This can make it extremely difficult to not only follow all of the ones in place today but to prepare our organizations for the upcoming regulations.
To help out, we reached out to our amazing Healthcare IT Today Community to see which healthcare regulations they foresee having a big impact on healthcare IT. The following is what they had to say.
Stephen Sofoul, SVP, Data & Decision Science Services at MultiPlan
A critical challenge lies in the shortage of experienced financial analysts or data analysts capable of effectively analyzing the wealth of information that the healthcare industry holds. As a result, the industry struggles to provide meaningful insights and harness the power of data to drive positive change. Price transparency is vital for making informed healthcare decisions, so enforcement of transparency-related policies will continue to increase. This will compel payers to take immediate steps to gain more visibility into their data to better inform that decision-making.
Mimi Winsberg, Co-Founder and Chief Medical Officer at Brightside Health
We have been in an uncertain time for regulation around telemedicine, and there are a few key trends to watch. The public health emergency (PHE) resulted in a temporary lifting of certain telemedicine regulations, but now post-PHE, we have seen that telemedicine is here to stay – particularly in behavioral health. Additionally, the DEA is now considering a telemedicine registry that will have implications for the kinds of treatments that can safely be delivered using tech-enabled services.
Further, as artificial intelligence (AI) takes center stage, new regulations may be needed to disclose the nature and source of care dispensed. Just like nutritional information on food packaging, disclosures about what aspects of care are the product of generative AI versus what has human oversight can improve public trust.
Regarding medication, several new psychiatric treatments have been approved by the FDA, including Auvelity for major depressive disorder, the SAINT transcranial magnetic stimulation protocol for treatment-resistant depression, and Zurzuvae for postpartum depression. New drugs and delivery models are going to challenge what can be delivered over telemedicine and challenge the regulations of how in-person services are delivered. With that, I predict we will see an emergence of “click-and-mortar” services that combine technology and in-person care.
Finally, the current state of tech needs to be updated. We need to refine the Ryan Haight Act to develop a telemedicine registry that can safely prescribe controlled medication virtually. Further, state-by-state laws requiring in-person meetings between psychiatric nurse practitioners and psychiatrist collaborators should be reexamined as these can safely take place over video conferences. As a physician who is invested in complying with current regulations, I welcome clear regulatory guidelines from both the FDA and the DEA on these matters.
Steven Fitzsimmons, CEO at Freshpaint
There is a steady stream of privacy legislation being introduced and passed at the state level – WA, VA, CO, CT, UT, MA, CA – many triggered by the Supreme Court’s decision to overturn Roe v. Wade. While the intention is to protect the privacy of patients, most legislation is a very strict application of privacy that will impact healthcare providers and services.
The industry as a whole is going to be under a lot of additional pressure to protect patient data – even data they may not know they are collecting. It’s not just web analytics and ads that are an issue but even things like maps and videos hosted on a website. Many organizations are conducting a full analysis of their sites and some have found more than 50 tools that create privacy risks.
As healthcare systems and providers modernize (or build) their technology stacks, it will be more important than ever to prioritize privacy and to understand new regulations at the state level, from HIPAA, and from the FTC.
Lynne Rinehimer, Manager of Compliance Editors and Sales Engineers at symplr
There are several regulations that have been introduced in the last few years that organizations are struggling with as they seek clarification and make modifications to be in compliance. The No Surprises Act was signed into law in 2020 and took effect last year. Many hospitals, health systems, and health plans still don’t have employees trained and don’t have the proper policies, procedures, and tech tools in place to be compliant, even with the two years of runway that was provided by legislators. And with potential penalty fees of $10,000 per case of noncompliance on the line, this lack of preparation has dire consequences.
Another likely forthcoming requirement that will exacerbate the existing challenges: in the coming years, the US Department of Health and Human Services (HHS) will implement the provision for convening providers to incorporate projected costs from co-providers on an estimate for a care episode. This means providers will need to include good-faith cost estimates for other providers in addition to their own, based on the patient’s treatment plan. This type of document will require not only top-notch billing tools but also new levels of contractual collaboration between separate provider entities.
Another regulation healthcare organizations should be paying close attention to is the 21st Century Cures Act and its information-blocking requirements. At the end of June, the Office of the Inspector General (OIG) posted a final rule that amended the civil monetary penalties for information-blocking violations. Under this final rule, individuals and entities that violate the information-blocking requirements face a penalty of up to $1 million per violation. This final rule does not apply to healthcare providers but instead is directed at health information networks and health information exchanges, as well as developers of certified health IT. There will be a separate notice of proposed rulemaking directed at healthcare providers that should be coming out in the near future.
OIG has identified specific factors it will look to when prioritizing information blocking complaints including the extent/level of the information blocking, the harm caused, the number of those affected (patient and provider), its duration, financial losses, and intent. Providers can look to, and learn from the investigations conducted, and penalties imposed as they wait for the provider-focused final rule. All healthcare entities should review their policies and procedures and educate their staff to better ensure their information-blocking compliance. These activities should be multi-disciplinary, including representatives from the Compliance Department, Information Technology, HIPAA, and Legal.
Lastly, organizations should continue focusing on the Price Transparency Rule. Organizational compliance with the Price Transparency Rule has been slow, with a recently published report showing only 36% of hospitals reviewed were in full compliance. This finding, coupled with the effort by CMS to enhance its enforcement processes makes an organization’s focus on compliance more important than ever. As CMS has recently shortened full compliance timeframes, eliminated warning notices, and now automatically imposes a civil monetary penalty for hospitals that fail to submit a corrective action plan within 45 days, organizations need to better ensure they are making their standard charges public in a comprehensive machine-readable file, as defined by the Rule.
Jeanie Heck, Education Services at e4 Services
One change that significantly impacted the healthcare IT landscape was the restructuring of evaluation and management (E/M) codes by the AHA in 2023. This regulation shifted the previous three key elements of E/M codings to medical decision-making (MDM) or time. This regulatory change has continued to cause coding errors and confusion throughout the year.
The AHA’s aim was to reduce unnecessary documentation and streamline the coding process. From a coding and auditing perspective, the focus on the “why” behind the level-of-risk assessment became pivotal in determining the MDM level for each patient. Healthcare IT systems, especially EHRs, played a key role in supporting documentation with the use of macros, smart phrases, and templates.
However, EHR macros must accurately capture the patient’s condition on the day of the encounter. CMS recently provided guidelines for documentation using EHR macros and stresses the importance of supplementing them with enough patient-specific information to support medical necessity determination. Relying solely on EHR macros for documentation was deemed insufficient, highlighting the significance of accurate and individualized documentation in healthcare IT systems.
Mo Weitnauer, Chief Product Officer at MRO
ACOs Impacted by Change to eCQM One of the biggest regulatory changes ahead directly impacts Accountable Care Organizations (ACOs) and their quality reporting processes. ACOs will soon transition away from Web Interface to electronic clinical quality measure (eCQM) reporting. Beyond a new format, the rule requires reporting for three eCQM/CQM MIPS measures across all patients, not just a subset as in previous years. Preparation ahead of the mandatory deadline is crucial for success and ACOs with multiple EMRs will face unique challenges. This includes finding solutions for data aggregation, updating documentation and workflows, and ensuring consistent data collection. Three important steps to navigate the transition include:
- Implementing a best practice process
- Getting serious about data integrity and timeliness
- Identifying and closing gaps in quality measures
If I were a regulator for a day, I would provide additional ACO education and support teams to balance current reporting requirements with ACOs’ need to test outcomes under the new format. It is vital that new regulations support advancements in healthcare technology while also maintaining the highest standards of care.
Wayne Singer, VP of Regulatory at Darena Solutions
We are still eagerly awaiting the HHS Office of Inspector General’s long-overdue ‘disincentive’ final rule for healthcare providers who are information-blocking as per the Cures Act. Sadly, it will likely require monetary penalties to drive widespread information sharing with patients and to compel providers, health IT developers, and payers to fully embrace this new reality.
Cassie Choi, Co-Founder and COO at Pair Team
It’s exciting to see states like California requiring healthcare providers to participate in data-sharing exchanges to improve healthcare delivery. Unfortunately, because this is a large and new initiative, the data being shared is not quite in a place that makes it easy to use for the average healthcare provider. Even for digital health companies who can work to optimize the data being shared into action, we’re faced with issues like duplicate information and messy data that’s hard to use. There are interesting companies like Flexpa that are helping to streamline data sharing by putting the patient in charge of sharing their healthcare and claims data with any healthcare provider they want, instead of health plans gate-keeping it behind red tape.
Kyle Sherseth, VP of Revenue Cycle Solutions at Savista
The price transparency regulations enacted over the last few years have been touted as a way to give patients control over their healthcare costs and make informed decisions about their care. While there are pieces of the current and upcoming requirements that are consumer-focused, most have fallen short of achieving the stated goal and require modifications, including:
- Expansion from hospital-based care to ambulatory centers, freestanding providers, and standalone physician groups so consumers can see a wholistic view of options for their care
- Removal of data-only administrative requirements that create confusion for consumers
- The focus of regulations should be on requiring accurate, easy-to-use price estimation tools that allow patients to quickly evaluate options side-by-side
- Removal of separate requirements for payors and providers as the information often does not match and creates confusion
- With the exception of uninsured care, only payors should be required to provide patient-friendly cost estimation so consumers can easily review options side-by-side across all expected service types and care settings (e.g. physicians, hospital care, freestanding imaging centers, ambulatory surgical centers, etc.)
Despite their shortcomings, the current price transparency regulations are not expected to go away anytime soon, so hospitals should focus on providing accurate, defensible, and compliant data to the public while making the information easy for consumers to understand and digest.
Joe Ganley, Vice President of Government and Regulatory Affairs at athenahealth
There is no shortage of potential regulations that could impact health IT and more importantly our customers, from how we regulate artificial intelligence, to privacy, to telehealth to TEFCA, to information blocking (HTI-1 Rule from ONC). But it’s worth noting that perhaps the most important one is the proposed 3.4% cut to physicians who treat the country’s most vulnerable patients through Medicare. Every healthcare stakeholder needs to say out loud what we all know to be true—that the way we reimburse ambulatory clinicians under Medicare is fundamentally broken and in need of a major structural overhaul.
To create a stable payment mechanism for all front-line clinicians, I see enormous promise in H.R. 2474 – dubbed the “Strengthening Medicare for Patients and Providers Act.” If passed, this bi-partisan legislation would link the Medicare Physician Fee Schedule to the Medicare Economic Index, removing the ongoing need for provider groups and ambulatory physicians to beg Congress for yearly short-term solutions to reduce payment cuts. This act would result in more precise reimbursements and reduce overall Medicare costs by ensuring the continuous delivery of high-quality senior care, which can help reduce hospital admissions.
Olivia Currin-Britt, Senior Director, Client Success at Savista
I anticipate a future where digital mental health will be subject to stricter regulations. Currently, the FDA does not regulate most digital mental health products, nor does it oversee psychotherapy, whether conducted online or in person. This lack of oversight has led to numerous investigations into the overprescribing of stimulants and deceptive marketing practices. It feels as though we are navigating through uncharted territory, akin to the lawless days of the Wild West, without a regulatory agency or a group setting standards in place.
Tyler Wince, Chief Product Officer at Myndshft Technologies
The future of healthcare lies not in more paperwork but in intelligent automation. As regulations evolve to modernize and standardize the data exchange process between providers and payers, prior authorization automation emerges as a critical focus. This bridge we are building paves the way for a future where focused regulations harmonize seamlessly with streamlined operations, enabling care providers to redirect their focus to where it truly matters—patient care.
Michael Gould, Associate Vice President for Interoperability Strategy at ZeOmega
Regulations that have to do with patient cost transparency and prior authorizations – as well as certified interoperability – will have the largest impact on healthcare IT. Interoperability improvements that streamline processes and data exchange have great potential for savings and adoption of these standards is the necessary step to ensure benefits can be realized. Adoption of certified HIT has reached 96% in hospitals and this is a great foundation for improving prior auths and patient cost transparency. Regulators have a greater success rate when engaging industry experts to develop rules in health IT. Since emerging technologies have upsides and downsides, engaging experts in development and real-world testing can enhance the benefits, ameliorate the downsides, and also have a path to manage inadvertent or unanticipated consequences of applying these technologies.
Recently, several organizations have published positions on CMS rules that overlap in the area of prior authorizations. It will be important for CMS to consider these and the need to innovate to improve prior authorizations so that patients will have timely access to care and reduce the burden for providers and payers.
Andrew Harding, Co-Founder & VP of Customer Success at Rivet
Patients have never had more opportunity to manage their healthcare experiences as they do now. The movement towards healthcare consumerism and implementation of new legislation, such as the Hospital Price Transparency rule, has brought previously unavailable transparency into healthcare costs. The benefits of this legislation for patients are undeniable, however, for hospitals, it is getting harder and harder to balance administrative obstacles to meet consumer expectations and comply with evolving regulations. To maximize the benefits of the Hospital Price Transparency rule and provide patients with the “shoppable” experience they are looking for, hospitals need to implement the right solutions to provide up-front patient cost estimates and improve financial transparency while minimizing the administrative burden on the organization.
Naomi Schwartz, Senior Director of Cybersecurity Quality and Safety at Medcrypt
Today’s intricate technology landscape ranges from legacy devices lacking security to cutting-edge designs, all under the watchful eye of regulatory cybersecurity mandates. The FDA’s RTA policy, effective Oct. 1, 2023, demands comprehensive cybersecurity data in premarket submissions, streamlining reviews. Simultaneously, the eSTAR program’s electronic submission template necessitates full cybersecurity details, driving proactive collaboration and integrated security practices. Effective strategies include stakeholder collaboration, uniting champions for cross-group security cooperation, and ensuring collective responsibility for cybersecurity to achieve optimal and timely market entry while neglecting security shortcuts can lead to significant developmental delays.
Quite a bit to think about here! Thank you to everyone who took the time to give us a response and thank you to everyone who took the time to read this article! We could not do this without your support. Did we miss a regulation that you think will have a big impact? Let us know either in the comments down below or through sharing this article on social media!
< + > Beyond the Science by Gary Zammit – Life Sciences Today Podcast Episode 46
We’re excited to be back for another episode of the Life Sciences Today Podcast by Healthcare IT Today. My guest today is Gary Zammit, PhD,...

-
As I’m sure you know, times are tough. Wages have largely remained the same while prices have risen across the board – and healthcare is no ...
-
Solution Erases Long Phone Holds for Patients, Supports Overwhelmed Medical Front Desk Workers, and Improves Patient Access to Physicians A...
-
Announcement written by Zack Kanter, Founder and CEO at Stedi In February of last year, I gathered our engineering team in a war room. Chan...