Thursday, February 29, 2024
< + > How virtual care is evolving beyond traditional applications – with a hand from AI
< + > Generative AI in Your Desk Drawer: How to Get There
Previous articles in this series have shown how generative AI can be used for administrative and back-office functions in health care. Now we’ll look at how models are trained for these specific purposes.
Training Generative AI Models
Every industry has to develop domain-specific models, and health care has the extra burden of protecting personally identifying data. These requirements raise the question of when the general-purpose solutions offered by major tech companies are appropriate, where health care organizations can get large enough data sets to develop models, and how vanilla LLMs—or foundational LLMS—can be enhanced by narrow data sets from a health care provider.
Harman Dhawan, founder and CEO of Bikham, says that now there are “fairly cheap” LLMs that providers can build on and customize. Not only are there well-known options from OpenAI and Google, but some LLMs are open source.
Jean-Claude Saghbini, President of the Lumeris Value-Based Care Enablement business, says, “Vanilla LLMs can certainly be used within specific solution designs that allow you to constrain and control the output. But in all cases, the use of AI for back-office work requires organizational guardrails. Team members have to be trained on how to use AI responsibly, and that means deploying a change management process to train and adopt this technology safely and effectively. Privacy concerns are an important consideration, particularly when using publicly facing AI platforms.”
Seek AI helps customers connect their structured data to LLMs, according to founder and CEO Sarah Nagy. She says that “training data does not necessarily need to be large to be effective.”
She adds, “It is best to start small, employing just the most important datasets, when working with LLMs. One reason for this is to get used to the novel workflows resulting from LLMs. Once acquainted with these workflows, the organization can expand to additional datasets.”
Iodine Software, according to chief product and technology officer Priti Shah, has the necessary business associate agreements (BAAs) to get patient data from their customers. She says that 27% of all U.S. patient admissions flow through Iodine solutions, including real-time data.
When you remember that the now-discredited IBM Watson was trained on research papers, you can understand why using actual patient data is crucial.
Melvin Lai, senior associate at Silicon Foundry, says that use cases vary, but that “training on a dataset ranging from hundreds of gigabytes to several terabytes of text data should yield a well-functioning LLM. ChatGPT-3 was trained on approximately 45 terabytes of text data. Models focused on specific tasks or domains typically require less data to develop, but this raises the importance of curating the quality of input.”
Nick Stepro, chief product and technology officer of Arcadia, says, “As one example, a patient’s A1C may be formatted in many ways within an EHR. Training a model to identify those variables and consistently map them correctly ensures the most valuable and useful output. Programmers should train models to deliver an output in a specific format every time. This makes the application more reliable and dependable, providing the consistency users expect.”
SS&C Blue Prism, according to Anna Twomey, senior director of healthcare, develops a generational AI model as follows: They start with either a vanilla foundational model or one based only on medical records. In traditional machine learning parlance, the results of the models are called vector tables and consist of rules such as “six percent of the decision depends on age, eight percent on the presence of diabetes,” etc. So SS&C Blue Prism analyzes the clients’ own data to apply a customized vector table.
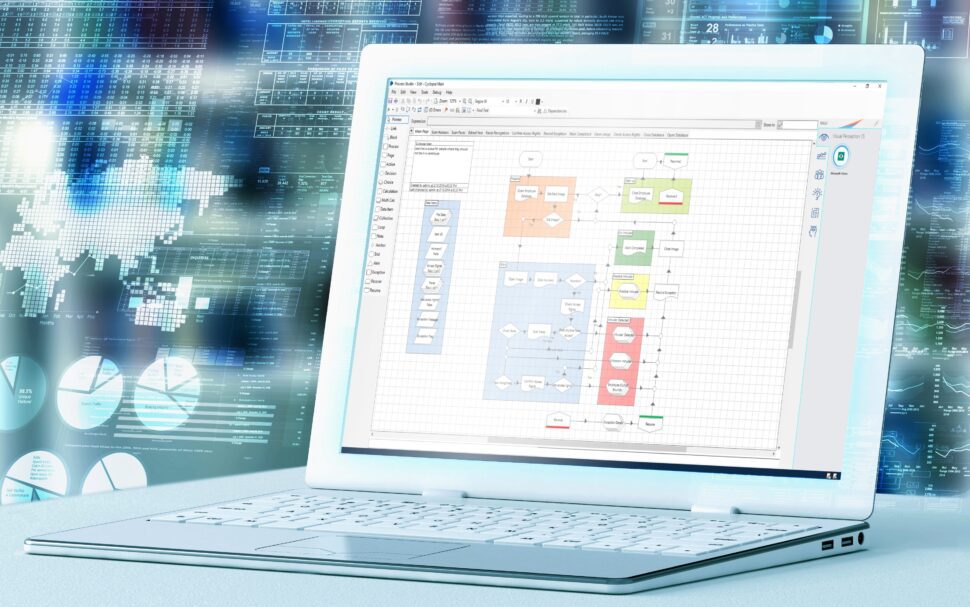
For audits and compliance, the tool can calculate metrics from the Healthcare Effectiveness Data and Information Set (HEDIS). These help an organization track how well it’s carrying out treatment, identify gaps in patient communications, and fill these gaps. Figure 1 shows a typical screen from SS&C Blue Prism.
Erik Barnett, North America Advisory Healthcare & Life Sciences Lead at Avanade, says that their clients normally run the service on internal data. For instance, staff can create a presentation by searching existing company documents, optionally accepting data from the Web as well.
Abhishek Sharma, principal of business transformation at Sagility, says they use generative AI to generate synthetic data for use cases around specific machine learning models for payers and providers when data is lacking. He advises health care institutions to combine generative AI with other digital assets and deep domain expertise to create a holistic solution.
Vignesh Ravikumar, partner at Sierra Ventures, predicts that industries will move over time to smaller, more specialized LLMs.
Chief customer officer Deirdre Leone at ContractPodAi believes that success for generative AI in contract development depends on domain-specific models, where specialized LLMs are trained to understand complex legal situations while also protecting sensitive patient information to avoid inaccuracies and misuse. “With this specialized information, a legal team can confidently draw up contracts and oversee them throughout their life cycle in more productive and efficient ways than before.”
Cameron Andrews, founder and CEO of Sirona Medical, writes to me, “Choosing LLMs is like hiring people: Some are smarter, some are more specialized, and some are more expensive than others. Health care organizations should focus on their IT infrastructure first, to ensure that they have the tools to pick, swap, combine, and tune LLMs easily and quickly or identify vendors and partners that do.”
Akshay Sharma, chief AI officer at Lyric, says they use a combination—what he calls an “orchestra”—of relatively Small Language Models (SMLs) that they can fine-tune and run on cheaper GPUs and even CPUs. Using their own data as input, they can develop special models, such as to reason and understand fraud, waste, and abuse, for coordination of benefits, and for other tasks in payment integrity.
By analyzing claims data and identifying patterns that may indicate fraudulent activities, healthcare providers can reduce the risk of financial loss and improve billing accuracy.
David Kereiakes, managing partner at Windham Venture Partners, says that organizations should include the end-users in the design process, using them for testing and opinions.
CitiusTech has recently announced a testing platform to evaluate generative AI quality, the CitiusTech Gen AI Quality & Trust Solutions. Sridhar Turaga, senior vice president, data and analytics, noted that, “Up to now, there have been no established technology-agnostic and platform-agnostic solutions that measure the quality and trust of healthcare generative AI, end-to-end. Approaches used in building and evaluating LLMs and foundation models are useful, but have not been designed specifically for healthcare.”
The CitiusTech solution enables clients to measure their models for accuracy, calibration, robustness, fairness, bias, toxicity, and efficiency. Multiple health care innovators beta-tested the approach, which can be integrated into existing MLOps, DataOps, and quality management solutions.
The final article in this series will take on the crucial issue of helping small providers, already strained past their limits to meet current patient needs, derive the benefits that this series has ascribed to generative AI.
< + > Three Key Takeaways From ViVE2024
Cybersecurity and the Change Healthcare outage dominated the hallway conversations at ViVE2024. AI was everywhere at ViVE2024, but companies were much more realistic with their productivity claims this year. In the exhibit hall, larger booths were more noticeable.
The three key takeaways from the ViVE2024 event for me were:
- Cybersecurity risk and the Change Healthcare outage was top-of-mind for attendees
- Vendors are being more realistic in their deployment of AI
- Larger booths are starting to appear in the ViVE exhibit hall
Lots of Cybersecurity Concerns at ViVE2024
Healthcare’s vulnerability, specifically to cybersecurity threats, was a top topic of discussion at ViVE2024. Although the importance of cybersecurity has been growing steadily over the past few years, the recent outage at Change Healthcare put cybersecurity on the minds of ViVE2024’s attendees.
In the lunch lines, the crowds between sessions, and in the aisles of the exhibit hall, attendees were talking about the vulnerability of healthcare’s technology infrastructure and the increasing threat posed by cybercriminals and hostile nations.
John Lynn and I cover this topic an upcoming topic of our Healthcare IT Today podcast.
AI Maturity on Display at ViVE2024
For the past two years, AI has been sprinkled like pixie-dust on everything – booths, marketing materials, and presentations. Vendors were applying AI in fantastic new ways (read: unproven) and making incredible claims on how the technology was going to help.
At this year’s ViVE2024 event, AI was still prevalent, however, the claims being made by vendors were much more realistic and attainable. This is a clear sign that the application of AI in healthcare is maturing…at least a little.
Larger Booths Creeping into the ViVE2024 Exhibit Hall
I remember the very first ViVE was mostly filled with 10×10 and 10×20 sized booths. At ViVE2024, the number of booths bigger than 20×20 was noticeable.
I’m not sure if this is a good or bad sign, but it says to me that we are entering a new phase in the evolution of the ViVE event. Having said that, despite the larger booth footprints, the ViVE2024 exhibit hall was still very manageable.
Wednesday, February 28, 2024
< + > How AI and FHIR can help reduce sepsis mortality rates
< + > NIST updates Cybersecurity Framework with Version 2.0
< + > Generative AI in Your Desk Drawer: A Wealth of Uses
Previous articles in this series introduced the role of generative AI in the healthcare back office and examined its use in billing and revenue management. We’ll cover a lot of other uses in this article.
Patient Contact and Care Management
CEO Rahul Sharma of HSBlox says that the next version of its CureAlign platform will use generative AI to help improve the care management processes in its CareTracker module.
Many patients need reminders, if not actually coaxing, to come in for appointments. The CureAlign platform personalizes outgoing communication based on past interactions with the patient. Sharma says that message generators can take language translation services and the level of education into account.
Once a patient is engaged, the care team can prepare the personalized plan and put in place device monitoring and data collection. CareTracker will help to set up a large set of nonclinical and administrative steps, including medication reminders, appointment scheduling, scheduling check-ins for telehealth appointments, creation of alerts and notifications when things do not go as planned, prescription refills, and prompting for daily exercise under the care plan.
Harman Dhawan, founder and CEO of Bikham, says that generative AI can help you generate patient notes and summaries by capturing voice and inputs in a live environment. There is a spooky aspect to this, but as doctors and patients get used to it, care can be delivered more efficiently.
Caen Contee, CEO and co-founder of Wellplaece, says, “Generative AI technologies offer unprecedented personalization in patient management by analyzing comprehensive data, including case histories and social factors. This analysis enables the creation of tailored treatment and communication plans for each patient, ensuring that their unique needs are met.”
He adds that “by allowing insurance plans and policies to be queried through natural conversation, AI creates a more engaging and understandable experience for patients. This approach demystifies the often complex language found in healthcare documents.” The user interface can be represented through avatars and video, providing 24/7 access to information.
Abhishek Sharma, principal of business transformation at Sagility, treats communications as a “transaction,” and says that email automation is “fundamental to any back-office processing.” AI can determine where each email message should go, for instance with a curated response. Moreover, he suggests extending back-office automation to case triage, where advanced LLM classifiers can precisely identify the correct routing for cases, either as a downstream process or when misroutes occur.
Trent Peterson, director of product design and head of user experience at AdvancedMD, points out, “AI is available on-demand and is never impatient. It is never distracted or preoccupied and never has something better to be doing. When done right, the user experience can be personal, flexible and intuitive.” When a patient explains their problem, a chatbot with a human-sounding voice can pose intelligent questions such “How severe is your pain? Can you describe it on a scale of one to 10?” and “Does tomorrow at 10 AM work for you?”
The AI service will finish by sending a personalized confirmation email such as, “We understand you are in a lot of pain and we have prioritized your appointment.”
Going further, Peterson expects AI agents, with access to all the patient’s clinical and financial information, to answer questions and even complete tasks on behalf of the patient. Additionally, AI is now being developed that, with permission, can “see” the user’s screen, and can take temporary control of the user’s mouse and keyboard. In health care, this might be used to show the user how to use the practice’s website and find needed information or complete an unfamiliar task.
Christine Duncan, manager, product management at AdvancedMD, says that generative AI can also assist in automating workflows that reschedule and cancel appointments and that manage waitlists. AI can also predict the probability that a patient will not show up for their appointment, or will cancel at the last minute. Going further, the AI can help explain the factors that make a missed appointment or late cancelation more or less likely. This enables front office staff to take extra steps for patients with these factors, to decrease the number of open time slots within their provider’s schedule.
Call Center Support
Imagine you are taking calls at 10:00 PM, and a person calls in to say they are experiencing chest pain. Wouldn’t it be great to have access to a senior cardiologist? How about a dozen senior cardiologists? AI can provide comparable support.
Doug Ross is vice president, US head of generative AI at Sogeti, part of Capgemini. During the next few months, they will be able to provide call centers with this kind of support, as well as administrative help, such as checking patients’ insurance coverage.
Dr. Rowland Illing, chief medical officer and director of global healthcare and non-profits at Amazon Web Services (AWS), suggests use cases for call report summarization and agent performance assessments. For example, generative AI tools could analyze a call transcript to highlight areas for improvement.
Jean-Claude Saghbini, President of the Lumeris Value-Based Care Enablement business, writes, “There are various methodologies that use existing, foundational LLMs while restricting the answers to be from prescribed data sets. An organization may have massive amounts of documentation and data that enable call center staff to search and provide answers to a member’s question. But unlike when you use the open version of ChatGPT, techniques can be employed on existing LLMs to provide direct answers to the questions asked while restricting the answer to being produced from the organization’s own data.”
Other Use Cases
In late 2023, Avanade started to offer Microsoft-based generative AI services that support admissions and discharges, which require staff to pull together a dizzying set of patient requirements and history. Avanade, a joint venture of Accenture and Microsoft, works with clients to employ Microsoft’s service.
Doug Ross is vice president, US head of generative AI at Sogeti, part of Capgemini. He says that additional back-office use cases include prescription guidance and prescription adherence. Capgemini works with several clients whose chatbots notice whether a patient has picked up their meds and then generate questions to ask why they haven’t: Are they deterred by the medication’s effects? Do they have difficulty taking the pills? These enterprises can then identify available substitutes, along with adverse interactions.
Melvin Lai, senior associate at Silicon Foundry, mentions that generative AI has many uses in pharma: “A well-designed protocol plans every level of the clinical trial, giving detailed consideration for components like design consistency, patient or site burden, and diversity and inclusion requirements. Exploiting successful prior trial protocols can be helpful in this process, but such information is buried in hundreds of pages of historical protocol documents and remains largely untapped. Generative AI can analyze this wealth of information and identify the key patterns, cost-saving opportunities, and streamlined operations to create new protocols for future clinical trials.”
WNS’s data capture and processing platform, Skense, underlies health care activities ranging from medical summarization and simplified bill review to scientific research. Skense ingests both structured and unstructured data, generates contextualized information, and creates structured datasets for business analysis and consumption by downstream applications.
According to Dr. Gauri Puri, head of healthcare and life sciences at WNS, Skense is already being used for clinical decision-making, as well many use cases discussed in this series, and others such as nurse reviews.
She writes, “Payers use AI not only to review claims history, but also to combine claims data with other reference datasets (such as lab, historical, and disease datasets) to build predictive models that forecast a member’s service consumption patterns. This is helping payers build personalized plans for every member. Pharma companies employ AI to create models using claims, research, and ‘omics’ data for precision medicine.”
Two key areas of focus, she says, will be patient/member experience and clinical support and decision-making. Finally, she warns the organizations using AI to stay abreast of evolving regulatory guidelines.
Wellplaece focuses on services for dental offices. According to Contee, they use generative AI to analyze resumes. He says, “AI systems can conduct a deep analysis to forecast the candidate’s future performance, evaluate their strengths and weaknesses, and rate them against specific job requirements.”
Priti Shah, chief product and technology officer of Iodine Software, talks of “clinical documentation integrity,” which can be found as a department in all health care systems. Iodine is used by nurses and by staff responsible for clinical documentation integrity to identify inaccuracies and prioritize which cases to review. The company has based its applications on its AI engine since its founding, and is now integrating GPT-4.
She says that an LLM can help give a better summary of what happened since the last time a physician reviewed a record. She says that AI explainability is important, providing background data to back up what the AI tool is saying.
Ryan Hamilton, chief product officer of MacroHealth, advises, “Organizations should look to AI to increase their business agility: their ability to predict, detect, and react quickly to changes in the environment.” MacroHealth talks about “intelligent health markets” and uses generative AI to improve savings and efficiency.
Nick Stepro, chief product and technology officer of Arcadia, says generative AI can aid data entry and management.
Axuall aggregates clinical data for applications that use generative AI to reduce onboarding time and solve other workforce issues. CEO Charlie Lougheed writes to me, “For AI to provide solutions that health systems can act upon, it must be provided with strong, up-to-date data. Inadequate data could lead to a flawed AI recommendation and consequently to mistrust toward the tool.”
Sirona Medical provides AI-based services for radiology, where images rather than text are the key data. According to founder and CEO Cameron Andrews, there is no follow-up for more than one-third of all incidental findings in radiology. He says, “Generative AI can parse radiology reports, identify follow-ups and critical findings, draft patient communications, and manage patient coordination and scheduling.”
Peterson says that the latest generation of LLMs have vision capabilities that allow them to extract paper-based EOB information, saving many hours of manual entry and related costs.
Strategic Solutions Group sees natural uses for generative AI in generating documents such as grant proposals.
The next article in this series will look at how to train healthcare LLMs.
< + > Healthcare Review of the Brother MFC-L6915DW All-in-One Printer, Scanner, Copier
When I first started doing IT in healthcare, I remember the thought and excitement around the paperless office. I remember seeing all those paper charts stored in the HIM office and thinking how nice it will be when everything is paperless. No more managing those charts and everything quickly accessible with a few keystrokes. While those paper chart rooms have disappeared, the paperless office hasn’t really come to fruition the way that many of us thought it may.
The reality in healthcare is that there’s still a lot of paper floating around the office. It turns out that paper is a great form factor that everyone can use with no training and has infinite flexibility. Everyone is familiar with the patient bringing in a stack of paper records that the clinical staff need to manage. We also see a lot of paper being printed in the office. In fact, one could argue that the EHR is a paper generating machine. One click and hundreds of pages can be printed. Ideally it happens electronically, but we know that the ideal option isn’t always available. Not to mention clinician’s need to print out patient instructions, prescriptions, consent forms, patient education, and more. Paper will be with us for a long time to come.
While I get that most IT people want to focus on the latest AI automation solution, it’s also important that IT staff select the right printers, copiers, and scanners too. The reality is that a broken printer can cause as much burnout and hassle for a clinician as clicks in the EHR. Making sure you have high quality printers and scanners in the right places is a key to ensuring happy staff.
 You may remember that we’ve reviewed a number of healthcare scanners over the years. This time we’re taking a look at the Brother MFC-L6915DW enterprise monochrome laser All-in-One Printer. I’ll admit that when I heard about the All-in-One Brother was sending me to review, I had a little bit of PTSD. When I first started in healthcare, I used a consumer grade All-in-One scanner and burnt them right out (My mistake, I was new). Let’s just say that the Brother 6915 All-in-One is nothing like those consumer grade All-in-One products that I inappropriately used in healthcare. It’s a workhorse that works in a variety of healthcare situations.
You may remember that we’ve reviewed a number of healthcare scanners over the years. This time we’re taking a look at the Brother MFC-L6915DW enterprise monochrome laser All-in-One Printer. I’ll admit that when I heard about the All-in-One Brother was sending me to review, I had a little bit of PTSD. When I first started in healthcare, I used a consumer grade All-in-One scanner and burnt them right out (My mistake, I was new). Let’s just say that the Brother 6915 All-in-One is nothing like those consumer grade All-in-One products that I inappropriately used in healthcare. It’s a workhorse that works in a variety of healthcare situations.
Let’s start by looking at the scanner. What’s great about the Brother 6915 All-in-One is that it has an incredibly robust, high duty scanner built in. It’s almost like Brother added the Brother ADS-4900W scanner to a printer. When you compare the two, the 4900 does 60 ppm vs 50 ppm for the 6915. In other words, both machines have more than enough speed and are built for the high volume scanning that’s needed in most healthcare situations. The 6915 also includes a legal-sized flatbed option for scanning with no need to buy a different model.
One thing I love about Brother products is that they all have the same display screen across their scanners and printers. So, if you’re using another Brother device in your office, you’ll be familiar with the display on the Brother 6915. I love the large 7 in display on the Brother 6915 which is great for handling any sort of workflow management on the device. Similar to the scanner we reviewed previously, it has a customizable user interface, uses the Twain driver, has a number of scan to options available including being able to do preset buttons to scan to a specific location or for a specific workflow. In fact, the screen is so big, you can even customize the logo on the screen.
 From a security perspective, the All-in-One doesn’t store any data on the machine. Many of us remember copy machines and scanners that stored data locally and then became a HIPAA violation when you go to replace and discard the old device. The Brother 6915 also comes with NFC authentication and can work with a wide variety of other authentication options. It also has SecurePrint where it waits for a pin to be entered to print. SecurePrint Plus can tie print jobs to a the user’s authentication. SecurePrint Advanced can be used to have the print jobs spool to a network drive. Plus, Brother works with TroyRx to handle secure printing of prescriptions on plain paper.
From a security perspective, the All-in-One doesn’t store any data on the machine. Many of us remember copy machines and scanners that stored data locally and then became a HIPAA violation when you go to replace and discard the old device. The Brother 6915 also comes with NFC authentication and can work with a wide variety of other authentication options. It also has SecurePrint where it waits for a pin to be entered to print. SecurePrint Plus can tie print jobs to a the user’s authentication. SecurePrint Advanced can be used to have the print jobs spool to a network drive. Plus, Brother works with TroyRx to handle secure printing of prescriptions on plain paper.
The printer itself does 52 ppm which should be more than fast enough for any healthcare situation. Many Brother machines use the same toner, so you don’t have to store a wide variety of toner cartridges for different printers and can standardize on one toner option. The device ships with a 11,000 page toner cartridge, but you can buy toner cartridges that do up to 25,000 pages. That’s a great option for organizations that don’t want to have to change the cartridge all the time.
 It’s funny to talk about copiers these days since a copier is essentially a scanner and printer, but this device can be used as a copier as well. Not sure there’s much needed to be said about the copier function, but Brother does have a cool ID copy feature that allows you to print both sides of the ID on one sheet of paper.
It’s funny to talk about copiers these days since a copier is essentially a scanner and printer, but this device can be used as a copier as well. Not sure there’s much needed to be said about the copier function, but Brother does have a cool ID copy feature that allows you to print both sides of the ID on one sheet of paper.
Brother does offer a number of interesting management features to monitor and support their devices. They have a field solution engineering team that can help a healthcare organization identify under and over usage so they can make sure they have the right devices deployed in the right places. Unlike some other device warranties, Brother provides a swap warranty where they send a replacement unit overnight as opposed to sending someone out to fix the broken device. You can clone the old machine when you go to swap it with the replacement device leading to less downtime for your users and happier staff. The device also provides the option to watch the syslogs for abnormal activity which can help in your cybersecurity efforts.
 One of my other favorite things about the Brother 6915 is that it’s extremely flexible. Just the standard device works great at a nurses station or at the front desk. However, the device can also have multiple trays added so that you can customize it for just about any workflow that you want. If you have a custom workflow and paper for prescriptions, you can add a special tray for that. If you need longer paper for a certain report, you can add a new tray for it. The ability to customize this device is what really sets it apart.
One of my other favorite things about the Brother 6915 is that it’s extremely flexible. Just the standard device works great at a nurses station or at the front desk. However, the device can also have multiple trays added so that you can customize it for just about any workflow that you want. If you have a custom workflow and paper for prescriptions, you can add a special tray for that. If you need longer paper for a certain report, you can add a new tray for it. The ability to customize this device is what really sets it apart.
All in all, I was impressed by the Brother 6915 in my usage. The device was easy to connect, customize, and use. The device is pretty large but not much larger than any laser printer you might get and this device has an ADF scanner, flat bed scanner, and copier built in as well. So the footprint isn’t bad when you consider all that it can do. I can see this being a popular device in healthcare where you often need a printer, high volume scanning, and a copier all in one location.
Tuesday, February 27, 2024
< + > Froedtert CTO talks AI scaling strategy, from 'small improvements' to 'hardest' last mile
< + > OCR settles its 2nd ransomware investigation, probably not the last
< + > Generative AI in Your Desk Drawer: Revenue Management
The previous article in this series introduced the topic of generative AI in the back office of healthcare. This article starts to look at healthcare generative AI use cases.
Is it any surprise that new technologies in health care pop up quickly in the area of reimbursements? Payments are the constant obsession of every manager.
Claims
Abhishek Sharma, principal of business transformation at Sagility, says that payers question why a doctor ordered an MRI instead of a less costly CT scan, and that precise details in the patient’s medical record and clinical demographic history have to be culled to justify the decision.
Dushyant Mishra, co-founder and CEO of RapidClaims, says that five to ten percent of costs in clinical institutions goes to billing and revenue management. The international ICD classification of diseases and conditions went from about 13,000 codes in ICD-9 to 68,000 in ICD-10. ICD-11 has already been formalized but is not in widespread use.
It’s really too much to expect a human coder to find the most appropriate code (translate: the code most likely to maximize reimbursement). Doing so requires checking historical records for symptoms, test results, and other data that the payer needs to validate a code.
Moreover, codes are routinely being added and deleted, and payers change their criteria for approving them. Mishra says that payers handle codes differently, some separating conditions and others preferring them to be combined. Ongoing training is required for human coders. It’s a textbook use case for AI.
Anna Twomey, senior director of healthcare at SS&C Blue Prism, lays out examples of subtleties that a human coder might miss. Sometimes, for instance, multiple medication pills are billed as a single dose. She says, “Additionally, the decision between bundled and unbundled procedures has significant impacts on billing. Human analysts may not always have the time to verify if all steps in a bundled procedure are accounted for, potentially missing charges. Generative AI, especially when combined with Robotic Process Automation (RPA), can meticulously analyze these procedures to ensure all relevant charges are identified and billed appropriately. In one organization, generative AI recovered more than a million dollars in missed (unbilled) dollars in a single quarter.”
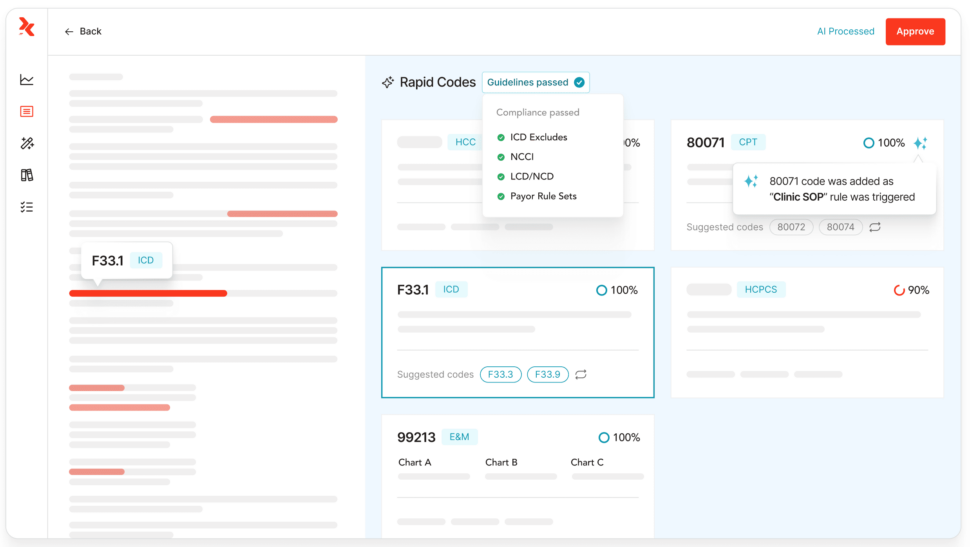
RapidClaims, which just announced a major funding round, focuses on automated medical coding. Mishra says that it doesn’t require a change to coders’ workflows. The efficiency provided by RapidClaims allows clinicians to increase the number of charts they process by 100% or more, leading to faster reimbursements. Figure 1 shows a RapidClaims dashboard.
My experience suggests that faster billing produces benefits for patients, too. How often have you received a surprise bill asking you to pay for some test or procedure that took place so long ago, you’ve forgotten it?
RapidClaims is focusing now on ICD-11 and thinks that their service will make the transition much easier for clinicians.
Akshay Sharma, chief AI officer at Lyric, describes rules for billing as a complicated set of layers of policies, with the Centers for Medicare & Medicaid Services (CMS), states, and private payers issuing large collections of clinical policy documents on a regular basis as new medications, diseases, and symptoms emerge. Thousands of pages of policies need to be evaluated as often as once a month.
“We’re capable of revealing the true impact of changes in documents longitudinally,” he writes. This approach, referred to as “reasoning based on unstructured text using language models,” uncovers specific extracts within the documents. These extracts are then presented to a human expert, who can offer feedback to help shape policies.
I suggested to him that it would make sense for the regulators to produce their own summaries, and he said he would like that to happen, but that they have no incentive to do so.
Lyric’s AI, based on a large corpus of knowledge built over decades, can also explain the adjudication decisions that have been made. Sharma writes, “The AI-based outputs are reviewed by experts who can provide feedback, which helps us improve the models. Specialized knowledge packs are built for payers to deploy the accurate setup.”
They also have plans to use generative AI for code generation. Sharma says, “This technology will assist in generating test cases and base code, ultimately enhancing the time to market for continually evolving policies.”
Iodine Software, according to Priti Shah, chief product and technology officer, uses AI to streamline utilization review in support of case management and documenting medical necessity, resulting in reduced insurance claims denials.
Prior Authorizations and Appeals
Next to billing, prior authorizations and appeals take up much of administrators’ attention. Doug Ross is vice president, US head of generative AI at Sogeti, part of Capgemini. He says the inputs to a prior authorization request vary for each type, and that generative AI can check whether all the necessary inputs are present in the request.
Experian Health released their AI Advantage program during the past year, aimed at large providers and offering various support for revenue cycle management. According to Clarissa Riggins, their chief product officer, one of their servies is denial triage: deciding which denials have the highest chance of a successful appeal.
Riggins says that getting approvals is not straightforward, but depends on a knowledge of how a particular payer will react, a “tribal knowledge” that staff learn over time. She says there are a lot of “if…then…else” decisions that generative AI can help you make. Such complexities arise when a patient has multiple insurance plans, or other sources of funding such as a charity.
Abhishek Sharma also describes how Sagility helps providers harness Generative AI to generate customized appeal letters, by summarizing requisite data points from a medical record. Conversely, Sagility aids payers by employing LLM-based classifiers for more precise identification and prioritization of incoming appeals, enabling the assignment of an expedited or urgent status when warranted.
Resource Management
Seek AI, according to founder and CEO Sarah Nagy, provides a natural language processing (NLP) interface that lets staff pose a wide range of questions with immediate responses, such as “How many patients did we see this week in comparison to last week?” Figure 2 shows a typical report from Seek AI.
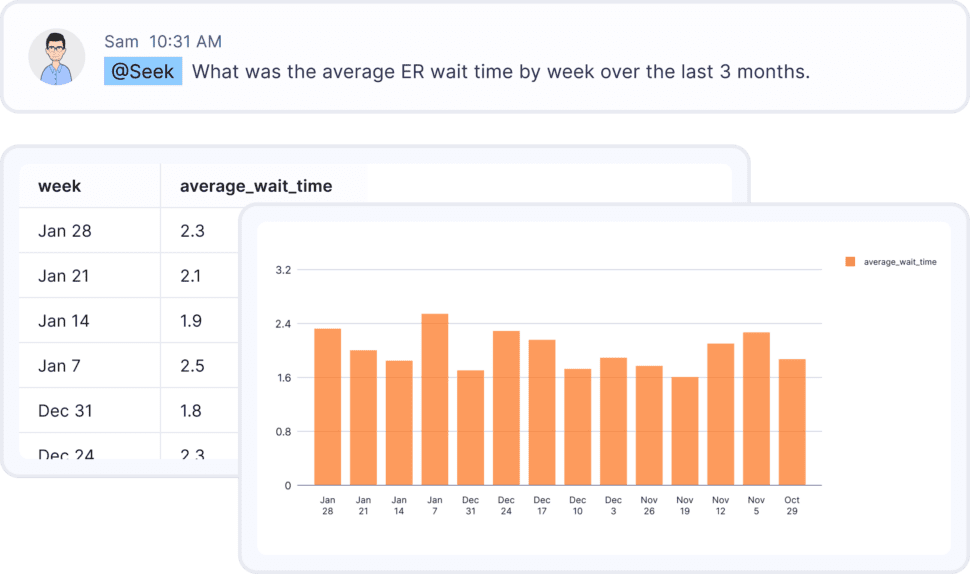
Nagy claims that Seek AI’s model is the world’s most accurate for typed language recognition for data.
Contract Generation
HSBlox provides a Value-Based Care Administration (VBCA) Platform that includes contract modeling and a contract builder. CEO Rahul Sharma explained to me that the platform has the flexibility to extract the pertinent data by processing existing contracts or digitization of traditional datasets. The company is building an interim stage in this process using generative AI. By training large language models (LLMs) on past contracts, generative AI can generate new contracts based on past patterns that can then be reviewed and finalized.
The platform passes that input through several stages. First, the contract modeler uses a combination of a rules-based engine and a query builder, built on Microsoft’s Power BI. Sensitivity analysis is performed by changing input variables, which determine the outcome of a decision given the combination of certain ranges and values of variables such as prices, coverage, and expiration dates. LLMs can analyze individual components of complex and lengthy contracts to extract those specific values.
Once the contract has been modeled, end users can use information from the contract modeler to build out the contract for different use cases. End users can also clone an existing contract from the library to edit and save as a new contract, based on sensitivity analysis done during the contract modeling stage. Sharma says, “This information can be extracted within seconds and presented with a simple-to-use workflow that allows users to finalize contracts within days.”
He emphasized that they are using a “data privacy vault” based on the IEEE’s recommended architecture for securely storing, managing, and using patient information by de-identifying fields. The de-identified data can safely be submitted to an LLM.
The next article continues to look at interesting uses for generative AI in the back office of healthcare.
< + > Bonus Features, ViVE Edition – February 27, 2024 – GE and Biofourmis collaborating on care at home, DeepScribe and AWS Health Scribe partnering, plus 20 other stories
Welcome to the weekly edition of Healthcare IT Today Bonus Features. This article will be a weekly roundup of interesting stories, product announcements, new hires, partnerships, research studies, awards, sales, and more. Because there’s so much happening out there in healthcare IT we aren’t able to cover in our full articles, we still want to make sure you’re informed of all the latest news, announcements, and stories happening to help you better do your job.
This edition is a special dispatch from the first days of ViVE 2024. There have been a lot of new research reports, products, and partnerships announced in Los Angeles. We wanted to try and cover as many announcements for the Healthcare IT Today community as we could. You can also listen to our ViVE 2024 Preview in Episode 134 of the Healthcare IT Podcast to get our take on the most important trends and topics on the agenda.
Partnerships
- GE HealthCare and Biofourmis are collaborating to support virtual care at home.
- DeepScribe is incorporating AWS HealthScribe in its platform and working with Amazon Web Services to scale large language models for healthcare.
- Clinical workflow automation vendor Lumeon was awarded Panda Health Partner Status.
- Tobacco cessation product 2Morrow has been integrated into the Spring Health platform for mental health management.
Product News
- AvaSure launched AvaSure Episodic, a virtual care tool for use cases such as admission, discharge, and specialty consults.
- CenTrack released Connect, a real-time location system for hospitals and health systems.
- Coeus Health launched Presence, a service for connecting front office staff with patients with support for 10 languages.
- Dolbey unveiled AI Assist, which offers generative AI for healthcare workflow automation.
- Engagement and payment vendor RevSpring updated Engage IQ with Quality of Visit and Quality of Payment metrics.
- Data security vendor Tausight is now integrated with Microsoft 365.
- VerifiNow launched PatientVerifi, a patient identity verification system for telehealth services.
Launches and Other Company News
- CancerX announced the 16 members of its inaugural Startup Accelerator.
- Axil Health launched; the clinical care management service provider formed as the merger of In-Clinic Rx and OnTrack Technologies.
- Online psychiatry service Lavender expanded to California, Nevada, and Oregon.
- CPSI unveiled TruBridge, its new branding officially effective Monday, March 4.
- Health and wellness vendor Vale Health launched in partnership with Froedtert & the Medical College of Wisconsin.
- Drug search engine Marketplace Search by Waltz Health is now available to Medicare health plans.
- The annual Xealth Digital Health Review noted preventive care programs had the highest levels of patient engagement among digital health programs, while surgery preparation programs had the highest enrollment.
Sales
- Vanderbilt Health Affiliated Network chose Quantum Health as its care navigation and coordination platform.
- Massachusetts-based Tufts Medicine selected Clearstep for digital triage and care navigation.
- WVU Medicine chose Hyro AI assistants for its websites and call centers.
- Self-insured employer health plan XO Health selected League to design its member experience platform.
If you have news that you’d like us to consider for a future edition of Healthcare IT Today Bonus Features, please submit them on this page. Please include any relevant links and let us know if news is under embargo. Note that submissions received after the close of business on Thursday may not be included in Bonus Features until the following week.
Monday, February 26, 2024
< + > Explainer: Thinking through the safe use of AI
< + > Generative AI to bring 'transformative change,' says Froedtert/Inception Health CTO
< + > Generative AI in Your Desk Drawer: Back Office Applications in Health Care
The Healthcare IT Today site has been promoting the use of powerful new capabilities in generative AI for clinical applications, notably the automatic generation of doctors’ notes after a patient visit. But there may be even more valuable uses of generative AI in administrative tasks such as billing, resource management, and contract writing.
Akshay Sharma, chief AI officer at Lyric, points out that 15-30% of health care costs in the U.S. are estimated to go to administrative burdens, while another 25-30% are consumed by fraud, waste, and abuse. Applying AI to administrative tasks could reap huge benefits.
And Harman Dhawan, founder and CEO of Bikham, says that eliminating human action from administrative activities is critical to making them scalable. He points out that health care has more trouble adopting new technologies than other fields because of the large sums of money involved, and because of compliance, but that the entry of smaller and newer companies into the field promotes innovation.
David Kereiakes, managing partner at Windham Venture Partners, says that despite the hype around clinical uses, the large clinical organizations with whom he consults are using generative AI a lot more in the back office. They feel that at this point, too much risk and liability surrounds AI use for diagnosis, notes, or other clinical tasks.
Kereiakes anticipates that it could take 15 to 20 years to see AI used widely for clinical decisions, although Caen Contee, CEO and co-founder of Wellplaece, anticipates the use of AI to help patients do self-diagnosis.
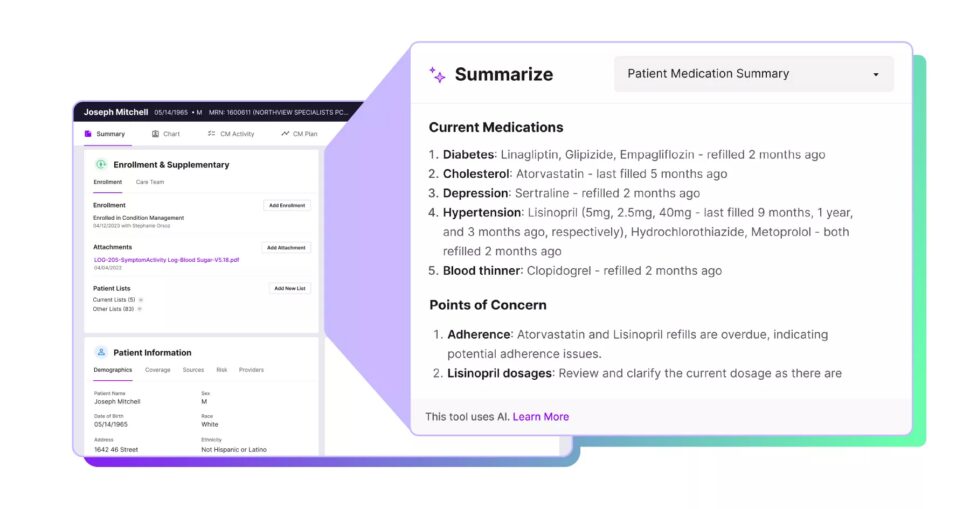
Nick Stepro, chief product and technology officer of Arcadia, also says, “Generative AI shows promise for clinical decision-making, but that application currently comes with higher risk. In the meantime, leveraging AI for back-office activities is a safer bet, and is an area of low hanging fruit where it’s being used a lot right now.” An example of Arcadia’s diagnostic summary is shown in Figure 1.
Dr. Gauri Puri, head of healthcare and life sciences at WNS, says that AI enables “a comprehensive understanding of patients,” which is crucial for value-based care and the modern focus on “wellness,” as well as to provide the retail-like convenience patients are demanding. Sources of data mentioned by Puri include clinical data, administration and operations, social determinants of health (SDoH), genomics, epigenomics and proteomics.
This article delineates the advantage of generative AI over earlier forms of AI and machine learning. We’ll look at several areas in health care where generative AI is in use, and discuss ways to make it widely available to small clinical organizations with few resources. We’ll also see how different organizations are training their models for maximum accuracy and value.
The Generative AI Advantage
The impacts of generative AI throughout society will be hard to assess for some time because it is so new and has become the darling of computer science so fast. Stepro describes the pace of change as “extreme.”
It’s hard to remember that ChatGPT was launched only near the end of 2022. In recent news, Google released Gemini, incorporating generative AI into a voice-enabled chatbot. One history credits Joseph Weizenbaum, creator of the classic Eliza program in the 1960s, for inventing the large language model (LLM).
But the key element of generative AI, the transform or transformer, was first proposed in a 2017 paper and only recently has supplemented the more traditional convolutional neural networks (CNNs) and recurrent neural networks (RNNs).
Traditional automation takes simple, linear tasks off of the hands of busy staff. Machine learning can go much further, uncovering useful trends that were previously unnoticed, and doing predictive analytics such as risk stratification of patients. But what can office staff get from generative AI?
While older forms of AI could produce simple numbers or charts, generative AI can produce complete documents. Although these documents need to be checked carefully by humans, the documents are often of higher quality than humans can produce on their own. First, they can adhere strictly to formats required by the recipient (such as for prior authorizations). Secondly, they are likely to capture obscure facts in electronic records that humans can easily overlook.
Stepro points out, “Humans are complex, and healthcare generates massive amounts of data, especially for patients with comorbidities. This increases the risk that important information could slip through the cracks. Generative AI, excelling in its ability to comb through the details, can help bring important insights buried in long patient histories to the surface. It can also help ensure that social determinants of health and other barriers to care aren’t missed, and that important information is considered in care plans.”
Dr. Rowland Illing, chief medical officer and director of global healthcare and non-profits at Amazon Web Services (AWS), says that traditional tools such as extract, transform, load (ETL) and intelligent document processing (IDP) cull data. “Now, organizations can use LLMs to normalize and transform the information to match the downstream databases where they want to store it. And instead of just asking very specific extractive questions, they’re able to do more complex tasks, such as asking the models to summarize the documents in a short paragraph or perform complex reasoning tasks on top of the data.”
Jean-Claude Saghbini, President of the Lumeris Value-Based Care Enablement business, identifies a “common archetype” for the use of generative AI: “To alter what had historically been a search into creating a direct path from a question to the applicable answer.”
Joel Ray, chief clinical advisor at Laudio and former chief nursing officer at UNC Rex Healthcare, emphasizes the importance of AI to simplify and reduce workload for frontline leaders at health systems, who play a vital role in ensuring high-quality care and stabilizing the broader frontline workforce. Currently, these leaders are overwhelmed by administrative burdens and growing team sizes. “AI and automation, focused on their ways of working, not only help boost their personal well-being and work satisfaction but also position them to focus more attention on engaging with and supporting their team members—thus helping to reduce burnout and retain staff at all levels.”
Upcoming articles in this series look at some of the many use cases that are taking place now, or might soon be feasible.
< + > CIO Podcast – Episode 69: Rural Healthcare with Dr. Michael Hasselberg
For the 69th episode of the CIO podcast hosted by Healthcare IT Today, we are talking to Dr. Michael Hasselberg, PhD, Chief Digital Health Officer at University of Rochester Medical Center (URMC) about his organization’s alliance to expand healthcare access to rural communities! We kick this episode off by diving into what problem inspired Hasselberg to start this project. Then Hasselberg goes into detail about all of URMC’s partners in this project and what their roles are and a partnership that will surprise you. Next, we get into the uses of the tools – what care they can and cannot provide. We then expand outwards to discuss the other digital health efforts URMC is doing. Next, we discuss the technology/initiative that Hasselberg has been keeping an eye on that he believes will benefit healthcare organizations. Finally, we wrap up this episode with Hasselberg passing along the best piece of advice he’s been given.
Here’s a look at the questions and topics we discuss in this episode:
- What was the problem you identified that pushed URMC to expand healthcare access to rural communities?
- Talk about all the partners that came together to make this happen.
- Who’s doing what with this first-of-its-kind alliance?
- What kind of care are you able to provide using these tools? What care can’t you provide?
- Outside of this alliance, what other digital health efforts is URMC doing?
- What’s a technology or initiative that you’re keeping an eye on that you think will be a benefit to healthcare organizations?
- What’s the best piece of advice you’ve been given in your career?
Now, without further ado, we’re excited to share with you the next episode of the CIO Podcast by Healthcare IT Today.
We release a new CIO Podcast every ~2 weeks. You can also subscribe to the Healthcare IT Today podcast on any of the following platforms:
NOTE: We’ll be updating the links below as the various podcasting platforms approve the new podcast. Check back soon to be able to subscribe on your favorite podcast application.
Thanks for listening to the CIO Podcast on Healthcare IT Today and if you enjoy the content we’re sharing, please rate the podcast on your favorite podcasting platform.
Along with the popular podcasting platforms above, you can Subscribe to Healthcare IT Today on YouTube. Plus, all of the audio and video versions will be made available to stream on HealthcareITToday.com.
We’d love to hear what you think of the podcast and if there are other healthcare CIO you’d like to see us have on the program. Feel free to share your thoughts and perspectives in the comments of this post with @techguy on Twitter, or privately on our Contact Us page.
We appreciate you listening!
Listen to the Latest Episodes
< + > Will AI’s Use in Healthcare be Regulated?
The potential benefits of Artificial Intelligence (AI) in healthcare are substantial. AI-powered chatbots can help direct patients to the most appropriate care provider. Ambient clinical voice can virtually eliminate the tedious task of charting for physicians. AI algorithms are can flag radiology images that appear abnormal so that radiologists can prioritize their workload.
AI is advancing quickly. It will not be long before the technology is capable of doing much more complex tasks like diagnosing patients. Should AI be used for this type of work? Is the risk acceptable? These are the questions that are being wrestled with by product designers, data scientists, physicians, and government regulators.
Given the risks and implications, will governments opt to regulate the use of AI in healthcare? And if they do, what form will that regulation take? To get an answer, Healthcare IT Today turned to an expert – Caleb Williamson, State Public Policy Counsel at the Connected Health Initiative, a group that works to clarify outdated health regulations and incentivize the use of connected health technologies.
Legislators are keen to know more about AI in healthcare
According to Williamson, governments at all levels are actively seeking to learn more about the use of AI in healthcare to help inform their decisions on potential regulations.
“Agencies and governments are starting to create task forces because they are recognizing there is a learning curve to AI,” said Williamson. “They are being quite honest with themselves and with their constituents by admitting there is a knowledge gap. They want to be quick to learn, but slow to regulate.”
Williamson hopes that regulators will learn that there are different risk levels to AI’s use in healthcare. Low-risk applications of AI in healthcare include process automation for revenue cycle management, crafting more personalized messages to patients, etc. High-risk applications include the use of AI to diagnose diseases.
To Williamson, this distinction is important because any forthcoming regulation should not, in his opinion, hinder the use of AI for low-risk applications that are helping healthcare organizations deliver better care to patients.
AI likely to be regulated
When asked this titular question, Williamson did not mince words: “Absolutely. Governments want to get involved.”
Governments want to protect people’s privacy – especially patient privacy. As evidence, Williamson cited the over 200 data privacy bills that were brought forward by state governments in the past few years, many of which include provisions specific to healthcare data use.
Williamson also believe governments want to put up guardrails on how AI is deployed in healthcare. He shared an example of a bill in the state of Georgia that would “prohibit the use of AI in the absence of meaningful human review.”
This sounds reasonable, until you consider that AI can be used on a website to direct patients to the closest clinic based on their language preferences, geography and medical needs. Having a person manually review that recommendation before being given to the patient would defeat the purpose.
This is exactly the type of situation that Williamson and the Connected Health Initiative are seeking to avoid. They are actively working with governments around the country to educate them on the nuances of AI and to avoid taking a blanket approach to regulating it.
Aiming for uniform, risk-informed regulations for AI
“We do not want to see a patchwork of bills and regulation that flood the country,” said Williamson. “We’re seeing that currently with data privacy. It is becoming more onerous not only for hospital systems, but also for companies who are building the new technologies. We want to make sure that this doesn’t happen with AI. We want to avoid stifling the use of this technology with a patchwork of regulations.”
Let’s hope that Williamson succeeds in his work to bring uniformity to future AI regulation.
Watch the interview with Caleb Williamson to learn:
- Why being informed on potential legislation is a competitive advantage for digital health companies
- How health IT companies can get involved in shaping future regulations
- What tools are available to track legislation that is being proposed
Learn more about the Connected Health Initiative at https://connectedhi.com/
Listen and subscribe to the Healthcare IT Today Interviews Podcast to hear all the latest insights from experts in healthcare IT.
And for an exclusive look at our top stories, subscribe to our newsletter and YouTube.
Tell us what you think. Contact us here or on Twitter at @hcitoday. And if you’re interested in advertising with us, check out our various advertising packages and request our Media Kit.
< + > Stellar Sleep Raises $6M to Help End Sleeplessness With the First Digital Sleep Therapy Platform for Chronic Insomnia
Stellar Sleep, which provides the first digital solution for chronic insomnia management, announced today a $6 million seed round, led by Initialized Capital with participation from Y Combinator, Lombardstreet Ventures, Switch Ventures, Moonfire Ventures, Scrum Ventures, 8vdx, and Goodwater.
More than 25 million Americans suffer from chronic insomnia – meaning sleep problems 3+ nights a week for 3+ months. The condition can lead to both mental and physical health issues, ranging from trouble concentrating to sleep apnea and heart attacks. For people suffering from chronic insomnia, superficial care advice (e.g. cutting coffee, reducing screen time, meditation, etc.) is not enough. Their insomnia is driven by deeper psychological challenges like unresolved anxiety, burnout, or depression. Stellar Sleep is a mobile app that helps users break the insomnia cycle using a proven, psychology-based methodology, and a clinical assessment of 500 users found it to be 50 percent more effective than sleeping pills.
This seed funding represents a significant milestone for Stellar Sleep, providing the ability to further expand capacity and reach. In addition, investments will allow for more comprehensive content and personalization of the user experience. “No one values sleep as much as those who can’t get it. The treatment options are so limited that these founders got trained as sleep therapists to treat themselves,” said Parul Singh, Partner at Initialized Capital. “Stellar Sleep is tech-enabled Cognitive Behavioral Therapy – true tech enablement of patient care that will make a meaningful impact on the millions of people who suffer from sleep disorders worldwide.”
Sleeplessness in America is on the rise, due to factors such as increasingly negative news cycles that keep people in a state of worry. Additionally, the shift towards hybrid-remote work arrangements has blurred the once-clear boundary between the “stress” space of work and the “rest” space of home. Collectively, these factors have caused more Americans to have recurrent sleepless nights than ever before.
The current American healthcare system isn’t well-equipped to deal with chronic insomnia. When superficial remedies don’t work, many people grappling with this condition turn to sleep medications, which often have dependency risks and are not meant for long-term use. Research shows that the most effective long-term solution for chronic insomnia is to address the root psychological causes, instead of just the symptoms.
Stellar Sleep was created when both Co-Founders (George Wang and Edrei Chua) personally suffered from insomnia for years and struggled to get care. Guidelines by physician organizations indicate that the best way to manage chronic insomnia is using a psychological approach called sleep therapy. This type of approach addresses the root cause of insomnia and helps the patient re-learn how to sleep well again. “What we found as we tried to get treatment for ourselves was that sleep clinicians are in such short supply – waiting lists of 6-12 months are common – that access to psychology-based care is a significant obstacle for the average person,” said Wang. “In addition to the waiting list, the cost and time commitment involved meant that out-of-pocket sleep therapy was out of reach for most. We founded Stellar Sleep with the goal of providing broad access to insomnia care via an app, a solution to a widespread public health problem that was previously unavailable to many.”
Stellar Sleep is the first digital solution on the market that goes beyond the surface-level symptoms and addresses chronic insomnia at the root. Here’s how it works:
- Users download the app, create an account, and complete an onboarding assessment that allows Stellar Sleep to understand the comprehensive picture behind their sleep issues. Users can also connect their wearables to provide an even more complete view of their sleep and well-being.
- Next, Stellar Sleep builds each user a custom, interactive program that guides them daily – and as needed in the middle of the night – to learn how to sleep well again. The program gets progressively more personalized based on the user’s sleep stats.
- Finally, Stellar Sleep helps users manage the user’s chronic sleep issues over the long run using psychology. This includes a combination of proven psychology techniques (e.g., CBT, acceptance and commitment therapy, motivational interviewing) that addresses the user’s root causes of insomnia (such as anxiety or burnout) and provides them with the tools to manage those root causes, so they don’t interfere with their day-to-day life and sleep.
“Stellar Sleep is the solution that we wish we had during our multi-year struggle with chronic insomnia,” said Wang.
Beyond the impact on physical and mental health, insomnia can be an incredibly isolating experience. Here’s a quote from Victoria, who struggled with insomnia for many years before finding Stellar Sleep: “I’ve had insomnia for about 5 years. I was at the point of desperation, willing to try anything. Insomnia feels very lonely. It’s 2 am and your spouse is asleep. You’re very alone with your anxious thoughts. It feels like you’re trapped and alone. After starting Stellar Sleep I’ve now started sleeping better for the first time in 5 years. I’ve gotten hope back that I can be normal.” With Stellar Sleep, anyone with chronic insomnia is now able to access personalized care at their fingertips and regain control over their lives.
About Stellar Sleep
Stellar Sleep offers the first digital solution for chronic insomnia management. 25 million Americans suffer from chronic insomnia, defined as sleep problems 3+ nights a week for 3+ months. Superficial approaches such as meditation or melatonin don’t help with chronic insomnia, which is typically rooted in deeper psychological challenges. Stellar Sleep was founded by two chronic insomnia sufferers who grew frustrated with the lack of resources available to address their condition. The app is grounded in Cognitive Behavioral Therapy (CBT), and in a clinical assessment of 500 users, Stellar Sleep was 50 percent more effective than sleeping pills. Subscriptions start at $60/month. Learn more at stellarsleep.com.
Originally announced February 6th, 2024
Sunday, February 25, 2024
< + > Canadian Smile's FHIR interoperability solution coming to ANZ
< + > Bonus Features – February 25, 2024 – 73% of digital health vendors use FHIR APIs, 83% of clinicians think telemedicine is good for chronic condition management, plus 28 more stories
Welcome to the weekly edition of Healthcare IT Today Bonus Features. This article will be a weekly roundup of interesting stories, product announcements, new hires, partnerships, research studies, awards, sales, and more. Because there’s so much happening out there in healthcare IT we aren’t able to cover in our full articles, we still want to make sure you’re informed of all the latest news, announcements, and stories happening to help you better do your job.
News
- U.S. Reps Mike Kelly (R-PA) and Bill Foster (D-IL) introduced the Patient Matching and Transparency in Certified Health IT (MATCH IT) Act of 2024, which would standardize the way demographic information is entered into certified health IT products and ensure more precise patient matches.
- Fourteen professional healthcare, life science, and consumer organizations formed the Digital Health Collaborative to advance evidence and value in digital health technology.
- The 29 members of the EHR Association shared concerns with ONC about upcoming deadlines for Certified EHR Technology deadlines given the complexity of needs specified in HTI-1 and beyond.
- Median hospital margins hit 5.2% in January, according to the latest data from Syntellis. That’s the highest that margins have been in about two years.
Studies
- More than 90% of healthcare executives agree that AI capabilities are expanding and will improve their organizations, according to Accenture’s Technology Vision 2024 report. That said, 69% of consumers want healthcare orgs to develop guidelines on privacy, ethics, and standards for using AI.
- A survey published in JAMIA found 73% of digital health vendors are using standards-based FHIR APIs when integrating with EHR systems. The news isn’t all good, as ONC noted in a blog post, as 68% of vendors are also using some form of proprietary APIs as well.
- A report from Hospital for Special Surgery found ChatGPT provided responses to patients’ questions that were easier to understand that medical literature – but also less comprehensive.
- Roughly 83% of clinicians agree that telemedicine is effective for managing chronic conditions, according to a SteadyMD survey.
Partnerships
- Instacart is now integrated with Pack Health, the patient engagement program from Quest Diagnostics.
- Dandelion Health has partnered with The SCAN Foundation to incorporate SDoH data on older adults into its data sets training clinical AI models.
- Clearwater is partnering with 25m Health to develop a cybersecurity and compliance program for health tech startups.
- Family caregiver education platform Trualta is now available through PointClickCare’s Marketplace.
Product and Company News
- Authenticx introduced a generative AI tool for summarizing recorded customer conversations.
- Trilliant Health released Network Explorer, which analyzes physician referral patterns and network performance.
- Edifecs said it will now enable compliance with CMS Interoperability and Prior Authorization Final Rule.
- Provider network management vendor Medallion launched a one-day credentialing solution.
- Health information network Availity issued five principles for the responsible use of AI.
- X-trodes receives FDA 510(k) clearance for Smart Skin, its wireless wearable for monitoring brain, heart, eye, and muscle activity.
- Experity announced its 2024 Limelight Awards at its annual Urgent Care Connect conference.
Sales
- WellSpan Health chose Biofourmis to support its bundled payment program for post-acute care at home.
- Texas-based community health center Healing Hands Ministries selected Sunoh.ai.
- California-based HIE entity Serving Communities Health Information Organization is using NextGen Healthcare’s Mirth interoperability solutions.
- Mental health service provider Brightside Health expanded Medicare and Medicaid coverage with payers in more than a dozen states.
- The Foundation for Chiropractic Progress selected AXYS for data management and integration.
- Ohio-based insurer Medical Mutual chose Strive Health to deliver value-based kidney care across all lines of business.
- Substance use treatment provider Flyland Recovery Network chose iPad software for in-room patient engagement, education, and entertainment from Volo Solutions.
People
- Home care management solution provider HHAeXchange named Scott Schwartz as Chief Operating Officer and appointed Lori Harrington as Senior Vice President of Product.
- Cancer care cost management platform OncoHealth made three executive appointments.
- In-room digital marketing platform Lincata appointed Rick Carpani as President.
- Provider-payer data exchange platform Madaket Health named Megan Schmidt and Tim Suther to its Board of Directors.
If you have news that you’d like us to consider for a future edition of Healthcare IT Today Bonus Features, please submit them on this page. Please include any relevant links and let us know if news is under embargo. Note that submissions received after the close of business on Thursday may not be included in Bonus Features until the following week.
Stay tuned on Tuesday for a special edition of Bonus Features with news and notes from ViVE 2024!
< + > Are You Experiencing Data Chaos or Clean Identity with Your EMPI?
Identity management is one of the most challenging problems healthcare IT organizations face. For those not familiar with identity manageme...
-
As I’m sure you know, times are tough. Wages have largely remained the same while prices have risen across the board – and healthcare is no ...
-
Solution Erases Long Phone Holds for Patients, Supports Overwhelmed Medical Front Desk Workers, and Improves Patient Access to Physicians A...
-
Announcement written by Zack Kanter, Founder and CEO at Stedi In February of last year, I gathered our engineering team in a war room. Chan...