The following is a guest article by Venki Subramanian, SVP Product Management at Reltio
When data is missing, inaccurate, incomplete, or misdirected, it can have severe, sometimes life-altering impacts.
For example, in a survey by the Journal of the American Medical Association, approximately 1 in 5 patients who reviewed their electronic health record (EHR) ambulatory notes found an error–and 40% of these patients perceived the mistakes as serious, including mistakes in diagnoses, medical history, medications, test results, notes on the wrong patient, and sidedness.
Healthcare organizations are grappling with the challenge of siloed structured data – a predicament where crucial patient information is confined within disparate systems that do not communicate. This data segmentation hampers the holistic understanding of patient health and impedes timely and coordinated care delivery. The siloed nature of such data repositories can be attributed to various factors, including using different EHR systems, varying data capture standards, and a historical lack of emphasis on system interoperability.
The solution to these challenges lies in the adoption of interoperable data systems. Interoperability, the ability of different information systems, devices, and applications to access, exchange, integrate, and cooperatively use data in a coordinated manner, promises to dismantle these silos. It offers a seamless flow of information across platforms and stakeholders, ensuring that the right data reaches the right place at the right time. As the industry increasingly recognizes the importance of data interoperability, healthcare companies are poised at the cusp of a data revolution that could redefine patient care.
Fragmented Healthcare Data is Costly for Patients and Providers
Signed into law by President Obama in 2009, the Health Information Technology for Economic and Clinical Health Act (HITECH) mandated the adoption of Electronic Health Records (EHRs) across healthcare systems. EHRs are real-time, patient-centered records that make information available instantly and securely to authorized users. A significant oversight in the 2009 legislation, however, was the lack of a standardized framework for EHRs. The lack of standardization has led to today’s healthcare industry’s fragmented data problems. There are an estimated 500 vendors that offer some variation of EHR products, while the average hospital uses 16 different EHR systems.
Disconnected, non-standardized structured data in the healthcare industry presents a multifaceted problem that significantly impacts consumers and providers. Data fragmentation across healthcare organizations leads to many issues that degrade the quality of patient care and operational efficiency. These are just a few of the challenges created by data fragmentation:
- Suboptimal Patient Care: Clinicians are frequently unable to access complete patient records, leading to suboptimal clinical decisions and increased medical errors. The lack of data fluidity for patients means repeated tests, inconsistent health advice, and a disjointed care experience.
- Post M&A Data Integration: Integrating disparate data systems and ensuring continuity and quality of care after an M&A event is challenging. With many healthcare investors looking to ramp up M&A activities, the onus is on healthcare institutions to unify their patient data, avoid EHR duplication, and streamline operations.
- Financial Costs: The costs associated with redundant data processes and inefficiencies further strain the financial resources of healthcare institutions, already burdened by the need to provide cost-effective care.
- Compliance and Privacy Regulations: The healthcare industry is subject to strict regulations such as HIPAA in the US, and GDPR in Europe. Health systems, hospitals, and related providers must comply with 629 discrete regulatory requirements across nine domains and spend nearly $39 billion a year on regulatory administrative activities, while an average-sized hospital dedicates 59 full-time equivalent employees to regulatory compliance, over one-quarter of whom are doctors and nurses.
- Security Threats: Health data is a prime target for cyberattacks due to its sensitivity. Protecting this data from breaches and unauthorized access is a constant challenge.
Interoperability in healthcare aims to support managing health information across all systems and ensure that the data remains intact and unaltered during transit, preserving its meaning across various systems and settings. This capability is crucial for delivering high-quality, coordinated, compliant, patient-centered care.
The Prescription for Data: Healthcare-Specific Data Products
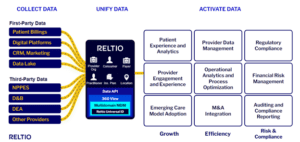
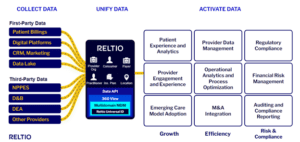
The advancement of data management and unification tools promises to be a game-changer for the industry, offering solutions specifically tailored to address the unique challenges of healthcare data. These tools include data products pre-built with healthcare-specific data models that significantly speed up interoperability.
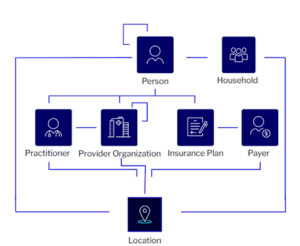
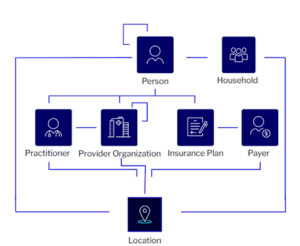
These tools accelerate deployment by utilizing out-of-the-box configurations and data models designed to standardize information for patients, practitioners, provider organizations, plans, payers, and households, allowing healthcare organizations to quickly reap the benefits of unified data. They streamline the often complex requirements definition and test case development processes by providing industry-specific, predefined implementation assets. This simplifies the initial setup and ensures that the configurations are optimized for healthcare data from the start.
Data enrichment is another critical area where these tools excel. With National Provider Identifier (NPI) data integration as an add-on, healthcare organizations can enhance their datasets with authoritative provider information, ensuring a more comprehensive view of the practitioner landscape. This integration is crucial for maintaining up-to-date provider directories and accurate billing information.
Prebuilt configurations for data cleansing, matching, survivorship, data quality, and user interface (UI) layouts further enhance the utility of these tools. They ensure that the data not only meets high-quality standards but is also presented in a user-friendly manner, making it accessible to non-technical users. The result is clean, accurate data that can be trusted for analytics and reporting.
Figure 1: Example of a pre-packed healthcare data model
Moreover, these sophisticated data management tools feed operational applications with trusted, timely, and accurate data. This is vital for day-to-day healthcare operations, where decisions must be made quickly and based on the most current and complete information.
Data management and unification tools are not just improving the quality of data in the healthcare industry but transforming information into a strategic asset. By delivering third-party data enrichment and ensuring the delivery of clean, accurate data to analytics and reporting tools, data products empower healthcare organizations to make informed decisions, improve patient care, and streamline operational efficiency.
Figure 2: How Healthcare Data Interoperability Unlocks Business Responsiveness
Furthermore, the application of Findability, Accessibility, Interoperability, and Reusability, or “FAIR” principles through these tools are revolutionizing data management. FAIR principles outline the guidelines for ensuring data can be effectively and efficiently used by all end consumers of data. Aligning with FAIR standards helps organizations effectively manage the growing volume, complexity, variety, and velocity of healthcare data. This approach facilitates findability, ensuring unique, searchable identifiers for data. Accessibility is prioritized, allowing data retrieval through standardized, open protocols ensuring compatibility across multiple systems. Interoperability and reusability are achieved through shared, broadly applicable data formats and vocabularies, enhancing data integration across multiple platforms.
The Interoperable Revolution: Business Responsive Healthcare Data
Digital transformation is essential as the industry pivots toward value-based care models, where the quality of data directly impacts the quality of patient outcomes. Providers are under pressure to ensure that every piece of patient information is accurate, accessible, and integrated—a herculean task that must be addressed. With the goal to have all Medicare payments processed through value-based care by 2030, the clock is ticking for providers to manage these data challenges head-on.
Achieving such interoperability requires robust modern data management and unification tools. These systems must navigate the complex landscape of varying data standards and formats and ensure compliance with stringent privacy regulations. They must be capable of cleansing, matching, and harmonizing data to create a single source of truth that is both reliable and readily accessible. Integrating technologies like entity resolution and master data management becomes indispensable in this context, providing the backbone for data governance and stewardship that underpins effective interoperability.
The evolving nature of healthcare delivery underscores the urgency of these advanced tools. The demand for real-time data exchange grows as care becomes more patient-centered and data-driven. The COVID-19 pandemic highlighted the need for timely access to accurate health data across different healthcare settings. Modern data management tools are not just facilitating interoperability; they enable business responsiveness in the healthcare industry to adapt to its ever-changing demands, ensuring that every stakeholder in the healthcare continuum can trust the data at their fingertips to be as current and comprehensive as possible. This trust is the cornerstone of the next leap forward in healthcare quality and efficiency.
 About Venki Subramanian
About Venki Subramanian
Venki Subramanian is Senior Vice President of Product Management, responsible for platform and industry solutions. Venki leads Reltio’s product strategy and works with the product and engineering teams to translate our long-term product vision into products and solutions that deliver value to our customers. He also focuses on building strategic technology partnerships and joint solutions.

 About Venki Subramanian
About Venki Subramanian
