 The following is a guest article by Bevey Miner, EVP of Healthcare Strategy and Policy at Consensus Cloud Solutions
The following is a guest article by Bevey Miner, EVP of Healthcare Strategy and Policy at Consensus Cloud Solutions
Investing in health equity is no longer just a moral obligation; it has become an economic imperative.
After analyzing the link between healthcare spending and disparities related to race, socioeconomic status, and gender, a Deloitte analysis concluded that health inequities account for approximately $320 billion in avoidable healthcare costs annually. If left unaddressed, this figure could reach $1 trillion or more by 2040, signaling an unsustainable crisis.
As the Deloitte study noted, prioritizing health equity can reduce unnecessary healthcare spending while improving health outcomes—saving dollars and, more importantly, lives. But achieving a measurable return on health equity investments requires an effective business strategy. It should be grounded in accessible technologies that can result in better health outcomes, thereby equaling lower costs. Additionally, a good strategy should include collecting the data needed to define and track progress toward this goal.
Communication Breakdowns
A recent survey of health IT leaders, commissioned by Consensus Cloud Solutions and conducted by the College of Healthcare Information Management Executives (CHIME), found that healthcare providers consistently face breakdowns in information sharing, especially when communicating with smaller facilities.
These gaps can be detrimental to care delivery and lead to higher costs, putting continuity of care and revenue at risk, particularly for providers treating the most vulnerable patient populations. In the survey, healthcare CIOs ranked breakdowns in care coordination as the biggest data-sharing challenge, followed by difficulties making (and following up with) referrals, finding patient information, and determining how and where to send information.
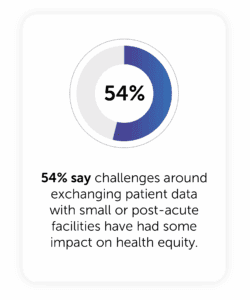
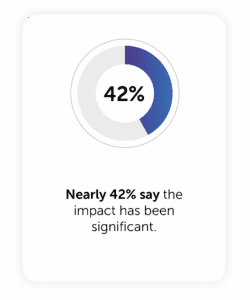
These barriers don’t just hamper operational and financial performance; they also impede equitable care. More than half of the survey respondents (54%) say the challenges surrounding access to patient data have impacted health equity, and nearly 42% say the impact has been significant. So, it’s no surprise that 62% of leaders surveyed say health equity is among their top priorities, and the majority of them (83%) agree that interoperable tech equity is critical to achieving health equity.
Disparities Across the Digital Divide
Without access to (or funding for) an electronic health record (EHR), many small, rural healthcare organizations rely on other modes of data exchange. According to the CHIME survey, nearly half of these facilities (46%) still rely on paper fax to share information with other providers. While 29% have moved to digital cloud fax, nearly 13% still pick up the phone, and 8% send a direct secure message. Once that information is received, it still has to be manually entered into the patient record, further complicating the workflow. While some users can share information within a few hours, the average data exchange timeline spans several days — sometimes up to a week or more.

These delays exacerbate the cost of information sharing challenges. For example, only 14% of post-acute care providers receive complete, timely, and usable data from hospitals, according to JAMA research. Half of these facilities don’t receive any information until the patient is already in their care, which opens the door to redundant tests, duplicate or interrupted medications, and other avoidable errors. Even more alarming, 76% say at least a portion of the data they receive isn’t even usable. As an example, patients are sitting in post-acute care facilities waiting for data to transfer so they can receive the care they need. This lack of continuity of care can worsen patient outcomes, cause unnecessary suffering, and increase healthcare costs.
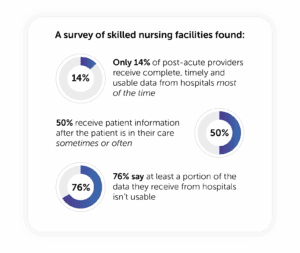
Source: “Information Sharing Practices Between US Hospitals and Skilled Nursing Facilities to Support Care Transitions,” JAMA, Jan. 14, 2021.
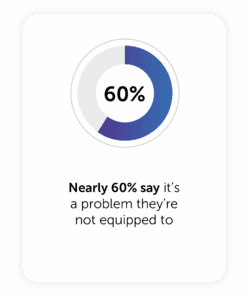
So, who’s responsible for solving this problem if care settings can’t equitably share information? Only 30% of large hospitals are working one-on-one with smaller providers to bridge these gaps, according to the CHIME survey, while nearly 60% say they don’t have the funding or IT resources to solve this problem.

Most respondents (50%) think it should be the federal government’s responsibility to fund this digital transformation, but that would require an unlikely multi-billion-dollar investment from CMS to upgrade every provider to interoperable EHRs and FHIR standards.
Since under-resourced facilities like substance abuse clinics, birthing centers, and critical access hospitals can’t afford these fixes on their own, we need a more practical solution.
Simple Solutions for Tech Equity
Fortunately, we can solve this problem without billions of dollars from CMS. Pairing artificial intelligence (AI) with digital cloud fax offers a pragmatic solution to level the playing field, leveraging a technology that most small facilities already use. By applying natural language processing (NLP) and machine learning (ML), these tools can extract data from unstructured documents like scanned faxes, handwritten notes, and images, and map this information into structured fields. These simple-yet-advanced technologies enable content to be securely transmitted and consumed by the receiving end patient record without manual data entry.
This pragmatic approach to tech equity unlocks numerous benefits for patients and providers, especially for vulnerable populations left behind in the digital transformation. By delivering data more efficiently and expeditiously, AI-fueled digital fax can:
- Enhance continuity of care
- Create better health outcomes
- Streamline referral management
- Enable providers to see more patients, which boosts revenue
- Reduce the burnout associated with administrative overload
- Improve billing accuracy
- Increase patient satisfaction
Moving from unstructured documents to structured, consumable data empowers efficiencies to support tech equity, which results in improved health equity. This measurable ROI gives providers more accurate and complete data to understand how to best tackle health disparities—improving outcomes for all.
No comments:
Post a Comment