Friday, June 30, 2023
< > UConn Health's CMIO discusses the challenging work of clinical workflow redesign
< > Iodine Software expands partnership with OpenAI
< > Process Automation Requires More than Just Technology
Healthcare sites are desperate to cut costs and reduce staffing needs through automation: As explained by Logan Lewis, Chief Operating Officer, EnterBridge Technologies, costs are increasing faster than reimbursements and few institutions in healthcare are expected to produce better profits over the next few years.
EnterBridge Technologies specializes in custom solutions to robotic process automation (RPA). This is not robotics in the sense of roaming machines, but simply software process automation for tasks such as getting prior authorizations, handling denials, and checking for suspect billing requests.
In this video, Lewis and Ryan Haubrock, Director of RPA Services, cover a wide range of topics in RPA. They address head on the resistance of clinical organizations who say “Our processes are unique and too complicated to automated” as well as “We just don’t have time and energy to make the transition.”
Lewis and Haubrock explain that good consultants can do the planning and implementation for their clients. “We do all the thinking for them,” says Lewis.
EnterBridge Technologies scrutinizes documentation for existing processes and works through multiple iterations of upgrading the documentation with the client to make sure it’s as accurate as possible. They have a robust development cycle that includes user acceptance testing on a substantial sample size.
Watch the video for more insights, such as the types of processes most suited to automation, the company’s standardization on a single platform, their views of the complementary roles of RPA and generative API, and how clinicians can render their claims departments much more efficient, possibly even turning them into revenue-generating units.
Learn more about Enterbridge: https://www.enterbridge.com/
Listen and subscribe to the Healthcare IT Today Interviews Podcast to hear all the latest insights from experts in healthcare IT.
And for an exclusive look at our top stories, subscribe to our newsletter.
Tell us what you think. Contact us here or on Twitter at @hcitoday. And if you’re interested in advertising with us, check out our various advertising packages and request our Media Kit.
< > Health Humor Fun Friday
Happy Friday everyone! It’s been a few weeks since we’ve done an edition of Fun Friday, so we need to remedy that now. For those not familiar with Fun Friday, it’s the time where we let our hair down and enjoy a little healthcare humor. I think you’ll enjoy these cartoons below.
#Surgery @JEFFsurgery @JEFFAortic @PascalJabbourMD @GianTorre610 @sminaev2015 @drroykim @VascularMD @NateEvansMD @BavariaMd @ScottGoldmanMD @alxbenevides @NeilFlochMD @LoggheMD @JJcolemanMD @NimeshDesaiMD @GilbertTangMD @Dr_Suse_ @ErbenYoung @pomyers @DrBabakAbai #RadialFirst pic.twitter.com/CTerFmi3sA
— Michael Savage (@DocSavageTJU) February 28, 2023
Surgeons are magicians! Just maybe not quite like this.
EKG #cardiotwitter https://t.co/OejnieK890
— Neil Floch MD (@NeilFlochMD) February 28, 2023
This is so brilliant. I always wondered about that stripe on Charlie Brown.
I drew up a diagram of where true comedy can be found. pic.twitter.com/NOh77f3lfa
— Dad Jokes (@Dadsaysjokes) May 31, 2023
As a Dad, I can really appreciate this important chart.
Always #believe in yourself 🔥 pic.twitter.com/sh1ub5EYLg
— Aaron Miri (@AaronMiri) June 25, 2023
This isn’t funny, but it’s inspirational. Thanks for the reminder Aaron.
Have a great weekend everyone and enjoy the 4th of July!
< > ML project to unlock siloed data on chronic diseases
< > e-Referrals system gains ground in Tasmania South Australia
Thursday, June 29, 2023
< > Health IT leaders can do better boosting access for underserved populations
< > OSF Healthcare using predictive AI to streamline care navigator workloads
< > NHS England appoints John Quinn as CIO
< > RCM: Fixing the Old and Adjusting to the New
Revenue Cycle Management (RCM) is like a one of those huge Lego sculptures. From the outside it looks one thing, but upon further inspection there are a million tiny little pieces that fit together to create the whole. Having a well executed RCM strategy is crucial to keep your organization running because it impacts everything. When things are simple and easy to pay for, patients are happy, the staff is happy, and you are most definitely happy. But if any part is misaligned, the whole sculpture can be disformed or even fall apart. So how do we improve? How do we make our sculpture be more realistic? The key lies in optimization. We need to be looking for areas that we can simplify to make everyone’s life easier.
But equally important to keep in mind as we optimize our RCM sculpture, as we optimize old practices, we need to prepare to adjust to the new changes. For example, for Legos any curves needed to be built using rectangles, because that was all that was available. To simplify this, Lego found ways to create arched pieces. But in optimizing the process, the old instruction manuals were now outdated and adjustments needed to be made.
To better understand ways that RCM can be optimized and how to best prepare for any needed adjustments, we reached out to our incredibly talented Healthcare IT Today Community for their insights. Below is what they had to share on this topic!
Kyle Sherseth, Vice President, Revenue Cycle Solutions at Savista
Revenue integrity programs aid in the identification and correction of process inefficiencies, thereby improving the overall revenue cycle. When done right, revenue integrity management supports the delivery of high-quality care, enabling providers to reinvest in staff, infrastructure, and technology, and ultimately improve patient outcomes. A successful revenue integrity program requires a multidisciplinary approach with the involvement of executive leadership and the establishment of a culture of transparency and accountability.
Ron Wince, Founder & CEO at Myndshft Technologies
Addressing inefficient prior authorization processes remain a crucial aspect of effectively managing the revenue cycle. Barriers to patient care lead to delayed procedures and denials that negatively impact healthcare providers’ bottom lines. Automating the process enables timely care while reducing operational costs creating a win-win for providers and patients alike.
Jordan Miller, Senior Medical Director of Dermatology at ModMed
U.S. doctors lose an estimated $125 billion in revenue each year to avoidable errors, such as incorrect patient or provider information, invalid or missing codes, duplicate billing and missing documentation. Integrated EHR and practice management systems with AI capabilities mitigate those mistakes because they can automatically suggest relevant ICD-10, CPT, and modifier codes. Automating coding and billing can also expedite the billing process and reduce administrative burden on clinic staff.
Huntley McNabb, Vice President at Nordis Technologies
Revenue cycle management communications can play a key role in rebuilding patient trust in healthcare, which fell sharply during the pandemic. Trust in information from doctors declined 23%, 21% for hospitals and 16% for nurses, according to Trilliant Health’s 2022 Trends Shaping the Health Economy. Just 23% of consumers completely trust the healthcare industry, according to Salesforce. To restore consumer confidence, providers need to leverage communications along the patient financial journey, from appointments to billing and payments. Consumers who trust healthcare organizations are 6X more likely to receive timely communications than consumers who don’t trust these organizations, Salesforce found. Using cloud-based communications platforms that enable mail, email and text messaging, providers and their RCM partners can personalize timely communications to increase engagement, improve patient financial experience and speed payments.
Clara Lambert, Director of Financial Navigation & Product Subject Matter Expert at TailorMed
Affordability is a major challenge for patients and healthcare organizations alike, and should be addressed as early in the revenue cycle as possible. Often, a patient’s financial distress is not recognized until it results in unpaid claims, which negatively impacts not just the patient, but also the wider healthcare system. For example, total patient statements with balances of $7.5K+ tripled between 2018 and 2021, while statements with balances of $14K+ nearly quadrupled in that time. These higher balances have created new challenges for providers and health systems, often resulting in dramatically lower collection rates. Providers must assess patients’ need for financial support on the front end of their intake process. With the help of technology, healthcare organizations can flag at-risk patients early on and help them locate and leverage financial resources before they receive a bill they cannot afford. Proactively addressing affordability ensures that bad debt and uncompensated care are avoided. This means more captured reimbursement for providers to bolster their financial health, as well as enhanced patient financial experiences.
Patrick Murphy, General Manager, TruBridge at CPSI
Leveraging advanced revenue cycle management software and analytics brings tremendous benefits to hospitals and health systems. By automating and streamlining billing, coding, and claims processes, healthcare providers significantly reduce administrative burdens, minimize errors, and accelerate reimbursement timelines. This not only improves cash flow, but also reduces costs associated with manual labor and inefficiencies. Adopting a patient-centric mindset is also crucial as organizations automate their revenue cycles. Healthcare providers should prioritize transparency and patient communications to ensure patients fully understand their financial responsibilities and are actively engaged in the billing process. The patient’s financial experience is remarkably enhanced with a streamlined revenue cycle process including clear and concise explanations of charges, available payment options, and personalized financial counseling. The two sides of revenue cycle automation (internal operations and patient engagement) work together to minimize confusion and potential disputes on the back-end for all stakeholders.
Shannon White, Chief Operating Officer at Ensemble Health Partners
It is critical to look at the RCM process holistically – too often provider organizations bring in technology partners that only address individual friction points within the revenue cycle, often leading to more fragmentation. One of the most fundamental ways that providers can optimize their revenue cycle for reliability of results and predictability of costs is by proactively conducting a comprehensive situational analysis of the challenges they may experience and the tools, partners and options they have if needed. Whether it is denial prevention measures, ensuring accuracy in capturing the complexity of services rendered or by improving utilization management – knowing the right actions to take and when to take them is critical to keeping the revenue cycle functioning efficiently. As far as technology and specifically AI’s role in improving revenue cycle management, it is certainly a critical component that can help analyze large quantities of data, identify patterns and predict payor behavior – but its most important value is in accelerating the human expertise, an element that remains a critical piece of an effective revenue cycle.
Amy Brown, Founder & CEO at Authenticx
The good news is that improving patient experience often has a compounding positive impact on improving cash flow and more efficient processes—thankfully, these business objectives are not mutually exclusive. The first step is to understand with a high degree of confidence the current customer experience and the root causes of negative experiences as well as the root causes of inefficient processes and barriers to cash flow. The best way to increase confidence is to collect statistically relevant data that is inclusive of leading indicators. We find that conversational data (call center conversations, including voice, text, chat, patient portal messages) is one of the best sources for leading indicators. It also provides a wealth of context that can be used to determine root cause analysis. For revenue cycle clients, listening to conversational data sources has been able to shed a light on the root causes of:
- Patient confusion on bills driving up inbound call volume
- User challenges with payment portals creating hurdles for customers trying to make payments
- Agent confusion and inconsistency in delivering instructions for payment or payment plans
Brooke LeVasseur, CEO at AristaMD
Value-based care shifts the focus of RCM strategies from charge capture to utilization. These models require providers to eliminate: Fragmented care that drives up costs. Requests for unnecessary or duplicate imaging lab work and tests. Delayed care that delivers poor outcomes for the patient. Technology can help. Referral management tools verify insurance, identify in-network specialists, and improve care coordination. Physician-to-physician consultations – or eConsults – enable primary care physicians to quickly treat lower acuity issues themselves. That means less care fragmentation, fewer unnecessary tests and faster diagnosis and treatment.
In an environment where specialists are in short supply, these tools prioritize face-to-face referrals while offering specialty care advice in the primary care setting. RCM data can identify areas where errors are made, like referring to an out-of-network specialist and opportunities to lower expenses, like accessing electronic consultations. PCPs can eliminate errors by verifying insurance before referring a patient, identifying in-network specialists and transferring patient information to avoid duplicate imaging and lab work – keeping costs low for the patient and the overall healthcare system. PCPs can lower costs and improve outcomes by leveraging eConsults to expedite specialty care access without the time and expense of referring the patient.
Laxmi Patel, Chief Strategy Officer at Savista
Given the financial and staffing challenges healthcare is facing today, globalization is here, and it’s here to stay. As healthcare organizations review their financial health and balance the scarcity of resources against their mission to deliver quality patient care, they must consider the utilization of global resources. A globalization strategy can reduce costs and help overcome staffing shortages, allowing for critical jobs to be made more meaningful and be retained domestically while more technical work is offloaded to expertly trained global teams.
Branden Barkema, Chief Revenue Cycle Officer at MedEvolve
Running an effective revenue cycle ultimately comes down to empowering your staff with the right tools/training and trusting them to execute. It’s important to consider the type of value you are creating for your organization. In other words, it’s not an RCM leaders’ job to do everything — it’s their job to see that it all is getting done. Technology is constantly evolving and change is part of everyday life as a leader. Effective leaders use their credibility to influence how their teams come to understand how technology and resources can be leveraged as effective tools to enhance process rather than viewing these things as a burden. If you have knowledgeable, skilled, and motivated employees who are placed in the best situation to succeed, your patients are sure to have a good experience. By effectively managing change, revenue cycle leaders can ultimately enhance the financial performance of their organization.
Lynn Carroll, Chief Operating Officer at HSBlox
The shift from fee-for-service to value-based programs requires a shift from the traditional claims-based revenue cycle to a whole-health model. In a more holistic health approach, where the emphasis is on the patient outcome, providers need to look for efficient allocation of resources, ensuring referrals are high-value and reducing the churn in getting the patient on the right care path.
Clarissa Riggins, Chief Product Officer at Experian Health
Changing payment models, such as value-based care, have a significant impact on revenue cycle management. In value-based care, reimbursement is based on patient outcomes and the quality of care provided, rather than the traditional fee-for-service model which incentivized cost reduction and increased utilization to improve margin. This shift requires healthcare providers to focus on preventive care, care coordination, and population health management. To adapt to these changes, providers can implement strategies like investing in data analytics to gain a better understanding of their patients to motivate wellness behavior, target community outreach, and track patient outcomes and performance metrics.
Understanding their community can help providers better target care and services to best meet those needs. By using data on consumers, providers can leverage insights for targeting preventative care and education making sure care coordination and limited population health resources are focused on the patients most likely to need and benefit from it. This can inform strategic focus for the services and specialties offered and will be in higher demand for the population providers service.
Also, insights help form more individualized and positive patient financial experiences. This part of the patient journey is vital because data shows a negative financial experience correlates to worse health outcomes. By reducing “no show” rates, implementing adaptive reminders, or identifying barriers to transportation providers can help ensure patients receive the care they need.
Additionally, another strategy is by partnering with employers to form a more collaborative and mutually beneficial approach to employee care and services, and a stronger united population health front. They can customize coverage and services, especially when they layer population health insights, in collaboration with the employers to create centers of excellence to best service their population needs.
So much to consider here!! Thank you to everyone that submitted a quote for us and thank you to everyone reading this article. We would love to hear from all of you as well! Comment down below or on social media with your thoughts on RCM optimizations and what adjustments you think need to be made.
< > What Are The Current Regulatory Changes And Compliance Requirements That ASCs Need To Be Aware Of In Their Billing Practices?
The following is a guest article by Isaac Smith, Billing, Coding, and Reimbursement Specialist at Medcare MSO
ASCs are types of medical facilities that are subject to stringent regulations. Each ASC is responsible for ensuring that they are in compliance with the numerous statutes and regulations that are in place at both the state and federal levels. These laws regulate everything pertaining to ASCs, from their day-to-day operations to the manner in which they are compensated.
ASCs must stay current on healthcare regulations that affect billing. New CMS and AMA guidelines, coding changes, and reimbursement methods have been implemented. To avoid penalties, maximize revenue, and accurately document claims, ASCs must understand these changes.
Understanding ASCs Regulatory Changes and Their Billing Practices
Outpatient surgery centers (ASCs) perform many surgical procedures outside of hospitals. Outpatient surgeries at these facilities are convenient, affordable, and specialized. However, ASC billing practices must be followed to ensure proper reimbursement and regulatory compliance.
Medicare Certification
ASCs must sign a contract with Medicare and meet its Conditions for Coverage (CFC) to be paid. ASCs must also meet Medicare’s Conditions for Coverage. From building layout to medical staff qualifications, these ASC regulations cover it all.
CMS publishes a State Operations Manual with interpretive guidelines for surveyors. Appendix L: ASC Interpretive Guidelines provides ASC-specific guidance. This document clarifies the Conditions for Coverage and advises ASCs on compliance.
Two other appendices apply to ASCs. Appendix I, Survey Procedures and Interpretive Guidelines for Life Safety Code Surveys, as well as Appendix Q, Guidelines for Determining Immediate Jeopardy, must be followed by all ASCs.
Medicare Payment Resources
CMS implemented an Ambulatory Payment Classification-based payment methodology in 2008. Visit the Medicare payment resources page on the ASCA website to learn about the changes that CMS has made to the payment system and ensure that your ASC is paid appropriately. The ASCA Medicare Rate Calculator displays national and local payment rates, as well as a chart comparing the rates charged by ASCs and HOPDs for the same surgical procedures, and additional information.
Medicare Quality Reporting
CMS mandates ASC quality data reporting. Future Medicare reimbursement will be denied to ASCs that fail to report. Quality reporting provides ASCA members with current requirements and resources to comply.
Emergency Preparedness
ASCs must have a CMS-approved emergency plan. As of November 15, 2017, ASCs are being surveyed on the new requirements of a September 2016 final rule. ASCs are required to evaluate risk, develop policies, procedures, and a communication plan, as well as train and test their final plan. Refer to the Interpretive Guidelines in Appendix Z of the State Operations Manual and this website for additional information. ASCA members can view an ASC-specific surveyor tag tool.
Other Federal Regulation Information
Affordable Care Act, Section 1557 Resources
The Federal Regulations section of ASCA’s website provides a starting point for understanding federal rules affecting ASCs, but it is not a substitute for a legal opinion from qualified counsel in this specialized area of law.
Compliance is the foundation of ethical and responsible ASC billing. For patient safety, fair reimbursement, and healthcare system integrity, regulatory bodies set compliance requirements. HIPAA, CMS, and state agencies regulate ASCs. ASC billing requirements include coding, documentation, privacy, and security.
Compliance Requirements for ASC Billing
ASCs should prioritize billing practices for compliance. This includes accurate and specific coding to reflect procedure complexity, detailed documentation to support medical necessity, billing and coding guidelines, and proper claims submission. These areas help ASCs reduce compliance risks and improve revenue cycle management.
Compliance Requirements for ASC Billing
ASCs can face serious penalties for not complying with regulatory changes. Updates and proper billing practices are crucial after recent enforcement actions and penalties. Audits, fines, repayment demands, and government program suspensions are enforcement actions. These consequences hurt ASCs financially and reputationally.
ASC billing compliance has many benefits. It promotes accurate reimbursement, reduces legal risks, improves patient safety, and builds trustworthiness and professionalism. Non-compliance risks ASCs’ financial and legal risks, patient trust, and long-term sustainability. Compliance protects ASCs and strengthens the healthcare system.
Maintaining ASC Compliance
Who performs these checks and tasks in your ambulatory surgery center? Besides the administrator! One person cannot handle this. Expecting one person to do everything increases the likelihood that nothing will get done and will cause problems when that person is unavailable (e.g., sick, vacation, leaving the position). To cover absences, other managers, leads, and staff should perform each check and task. Vendors will do some work. This starting task template spreadsheet can help you organize your checklist.
Overwhelming tasks and checks. Delegate, but monitor. Create tools to simplify and stay on track. If you fall behind even slightly, catch up quickly and figure out why and how to avoid falling behind again. Expect the unexpected, such as a leader’s absence or a natural or manmade disaster. Most importantly, treat your staff well. They’ll help your ASC comply year-round.
CPT and ICD Codes In Ambulatory Surgery Centers
ASCs use CPT and ICD-10-CM for diagnosis, procedures, drugs, and devices. ASCs must implement the latest ICD-11 diagnosis updates when they take effect. ASC Medicare billing does not require C-Codes like outpatient billing. Medicare reimburses drugs and devices differently.
ASCs billing Medicare should not use HCPCS II devices and drug codes. Use separate lines to report and bill each device or drug. Practolytics helps ASCs set up the right practices for documentation, coding, and billing. Coding and capturing all patient services can be overwhelming.
Regulatory Changes & Compliance: How Outsource ASC Billing Services Provider Can Help?
In the constantly evolving landscape of healthcare billing, ASCs (Ambulatory Surgery Centers) face the challenge of staying updated with the current regulatory changes and compliance requirements in their billing practices. To navigate these complexities successfully, ASCs can rely on the expertise and support of ASC billing services provider. Let’s explore the current regulatory landscape and how ASC billing services providers can assist ASCs in meeting their compliance needs.
Expert Knowledge of Regulatory Changes
ASC billing services providers understand current regulatory changes affecting ASC billing practices. They follow Medicare reimbursement policies, coding and documentation guidelines, HIPAA compliance, fraud, and abuse prevention, prior authorization, and state-specific regulations. ASCs can reduce errors and non-compliance by partnering with such providers.
Implementation of Best Practices
ASC billing services providers have extensive experience implementing billing best practices. They can help ASCs implement regulatory-compliant workflows, coding, and documentation. This improves ASC billing accuracy, efficiency, and compliance.
Dedicated Compliance Teams
ASC billing services providers often have dedicated compliance teams that monitor and address regulatory changes. These teams actively track updates and keep ASCs informed of compliance requirements. ASCs can benefit from dedicated resources and proactive compliance management by partnering with such providers.
Advanced Technology and Systems
ASC billing services providers use advanced technology and billing systems to streamline operations and improve compliance. They use robust billing software with regulatory guidelines, automated coding checks, and auditing functions. These technologies help ASCs bill accurately, reduce errors, and comply with regulations.
Ongoing Training and Education
ASC billing services providers educate ASC staff about regulatory changes and compliance. They hold regular sessions to update ASCs and their staff on coding, documentation, and industry best practices. ASC billing teams are informed and compliant.
 About Isaac Smith
About Isaac Smith
Isaac is a highly accomplished healthcare professional with over 13 years of experience in healthcare administration, medical billing and coding, and compliance. He holds several AAPC specialty certifications and has a bachelor’s degree in Health Administration. He worked previously at a large multi-physician family care and occupational health practice with two locations in northwestern PA and now works for Medcare MSO in the ICD-10 Editorial department to write articles about medical billing services. He enjoys sharing his knowledge and experience as a certified PMCC instructor. He has authored many articles for healthcare publications and has been a featured speaker at workshops and coding conferences across the country.
< > BurstIQ Acquires Business Intelligence Platform from Olive AI
The Partnership Elevates Evidence-Based Business Intelligence for Cost Savings, Efficiencies, and Quality Improvements
BurstIQ, a trusted leader in data-driven healthcare solutions, proudly announces the acquisition of Olive AI‘s business intelligence solution. This strategic move expands BurstIQ’s portfolio of innovative products, reinforcing its commitment to helping healthcare organizations navigate the complexities of data-driven solutions while maintaining strict privacy and compliance standards. The acquired solution, now known as LifeGraph Intelligence, further enhances BurstIQ’s offerings, revolutionizing how organizations see and use their data.
LifeGraph Intelligence leverages cutting-edge technologies such as Natural Language Processing, Machine Learning, and AI to extract meaningful insights from clinical notes and EMR fields. By connecting health systems’ quality, efficiency, and cost data with evidence-based content, including journal articles, guidelines, and recommendations, the platform empowers organizations to take action on opportunities related to cost, time, and quality improvements. The insights facilitate clinically meaningful discussions with physicians and enable organizations to take action to reduce unwarranted clinical variation system-wide.
“We are thrilled to add Olive’s business intelligence solution to our portfolio, allowing organizations to see and leverage their data in exciting new ways,” said Frank Ricotta, Founder & CEO at BurstIQ. “In the future, we plan to enhance LifeGraph Intelligence to address crucial healthcare challenges such as total cost of care reduction, quality measure reporting, clinical trial matching, and supply chain management.”
BurstIQ’s acquisition builds upon the success of Olive AI’s business intelligence solution, which delivered substantial savings to multiple healthcare systems. These savings range from $250 to $500 per surgical case, resulting in total savings of $2.1M to $10.5M per hospital per year. One health system even achieved an impressive $90M in savings over a five-year period.
This acquisition represents a significant milestone in BurstIQ’s mission to provide comprehensive, secure, and actionable healthcare data solutions. Equipped with this new technology, BurstIQ is well-positioned to continue helping customers unlock the full potential of their data, delivering trustworthy insights that drive cost reduction, improve efficiency, and enhance patient outcomes across health systems nationwide.
For more information about BurstIQ’s acquisition of Olive AI’s business intelligence solution and the launch of LifeGraph Intelligence, please contact BurstIQ or visit burstiq.com/lifegraph-intelligence.
About BurstIQ
BurstIQ‘s LifeGraph platform empowers organizations to connect and derive meaningful insights from any data source, enabling powerful business intelligence and hyper-personalized experiences. With the most private, secure, and trustworthy data fabric available, you can build a connected, continuously learning data ecosystem that helps you reduce costs, save time, and improve outcomes across your enterprise.
Originally announced June 13th, 2023
Wednesday, June 28, 2023
< > Survey: 1 in 3 patients comfortable with AI-led primary care
< > For Tempe AZ Public Health Means Being a 20-Minute City
The City of Tempe, Arizona, is using modern technology and an advanced infrastructure planning approach to enable people to make better health choices. This means ensuring everyone has access to fresh food, convenient transportation, and even adequate shade cover. It’s all part of their “20-minute city” initiative. To achieve their goals, city leaders are using a data-informed approach, enabled through GIS technology, to identify gaps in community infrastructure and planning.
Healthcare IT Today sat down with Dr. Stephanie Deitrick, Chief Data and Analytics Officer for the City of Tempe, to learn more about their public health initiatives and how it relates to being a 20-minute city.
Determinants of Health
According to the World Health Organization (WHO), there are many factors that affect the health of communities and individuals:
To a large extent, factors such as where we live, the state of our environment, genetics, our income and education level, and our relationships with friends and family all have considerable impacts on health, whereas the more commonly considered factors such as access [to health care] and use of health care services often have less of an impact.
Given this statement, its clear that improving health requires a holistic review of the factors that can make people and communities either healthier or sicker. For example, we know that access to fresh food and community services are important health factors that can be challenging for people who live and work in urban areas. The City of Tempe is addressing this challenge though its goal of being a “20-minute city” and is leveraging GIS technology to make data-informed development decisions.
Using GIS Technology for Healthier Living
In 2012, Kent Larson described the concept of a 20-minute city in a TED Talk. This concept has been adopted by many cities around the world, including the City of Tempe. The City has publicly defined their goal to create a vibrant mix of commercial, recreational, civic, and residential establishments within a 1-mile walking distance, 4-mile bicycle ride, or a 20-minute transit ride.
“Blending all the factors and all the requirements for a 20-minute city is very data-intensive,” explained Deitrick. “We needed to have a way to visualize all of this so that we can look for areas where there are gaps in coverage and to ensure optimal placement of shade, roads, and bike paths.”
The City of Tempe relies on GIS technology from Esri to visualize the data.
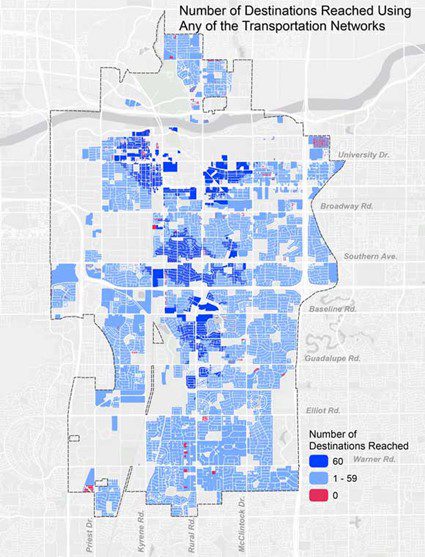
Source: https://www.esri.com/about/newsroom/arcuser/walkabletempe/
The map above shows the network analysis from the City of Tempe and the number of destinations, like grocery stores, that are reachable via walking, biking, and public transportation routes.
“We want to entice residents out of their automobiles and make use of other methods of transportation, which creates efficiencies in the transportation system and improved quality of life and public health,” explained Deitrick in a prior interview.
Watch the interview with Dr. Stephanie Deitrick to learn:
- Why the shade canopy is an important consideration for city planners
- The secret to being an effective GIS technology champion in an organization
- How they use wastewater data to improve community health
- Why an open-data approach can lead to unexpected benefits
Learn more about the City of Tempe at: https://www.tempe.gov/
Learn more about Esri at: https://www.esri.com/en-us/industries/health/overview
Learn more about GIS for Health at: https://www.healthcareittoday.com/gis-for-health/
Listen and subscribe to the Healthcare IT Today Interviews Podcast to hear all the latest insights from experts in healthcare IT.
And for an exclusive look at our top stories, subscribe to our newsletter.
Tell us what you think. Contact us here or on Twitter at @hcitoday. And if you’re interested in advertising with us, check out our various advertising packages and request our Media Kit.
< > Walmart seeks to make HIV care accessible at retail locations
< > How Automation Can Help Ease Healthcare Worker Burnout
The following is a guest article by Anna Twomey, Senior Director, Healthcare Providers – Americas at SS&C Blue Prism
With rising staffing shortages and burnout among healthcare workers, digital transformation will be key to overcoming these challenges and protecting patient care. It’s estimated that the U.S. could see a shortage of up to 124,000 physicians by 2033 and will need to hire at least 200,000 nurses per year to meet increased demand and to replace retiring nurses. The healthcare worker burnout crisis in this country began before the COVID-19 pandemic, but the public health emergency made the situation even worse as frontline health workers risked their lives to service others.
The pandemic accelerated the need for digitalization across industries, including healthcare. This was critical to delivering healthcare to patients who could not leave their homes due to various lockdown restrictions, forcing patients and clinicians to become more accepting of telemedicine.
Emergency rooms throughout the U.S. are overwhelmed by long wait times. Resource strain combined with the legacy infrastructures still being used in most health organizations have only added to these challenges. Tack on tightening regulatory procedures and you’re left with a healthcare system that is struggling.
How Artificial Intelligence and Other Tech can Help
Even when it comes to electronic health records (EHRs), an area where many countries are making strides, the issue of interoperability remains. This precludes the effective, timely, and secure transmission of patient data. While most health executives recognize the long-term benefits of digital transformation, many struggle with how to get started while under immense resource strain. For example, while the UK and Scandinavian countries are using digitization to help with margin pressures, the US and Australia are letting such pressures curtail the adoption of new technologies.
Intelligent automation (IA) has the potential to fill these gaps, unburdening healthcare workers so they can focus on the human side of healthcare, streamlining administrative tasks, improving patient access to care, enhancing patient engagement and experience, and enabling collaboration between healthcare professionals and organizations.
IA is a combination of artificial intelligence (AI), robotic process automation (RPA), business process management (BPM), and other complementary technologies that enable companies to advance workflows and streamline end-to-end processes. Digital workers can do routine administrative tasks, such as appointment scheduling, claims processing, and data entry. This frees up healthcare professionals to focus on complex, higher-value tasks, like patient care and research. Digital workers can operate 24/7, minimize errors and improve efficiencies by replacing manual processes. Again, that relieves overworked healthcare personnel from having to do these repetitive tasks.
AI and machine learning (ML) can analyze large amounts of healthcare data to uncover patterns and insights that can inform decision-making. For example, ML algorithms can help identify patients who are at high risk for certain conditions, allowing healthcare providers to intervene earlier and potentially prevent more serious health issues as well as save costs and time down the line. These technologies can also be used to develop predictive models for hospital readmissions, disease progression, and patient outcomes, allowing providers to deliver more personalized care and improve outcomes.
BPM can help healthcare organizations streamline and coordinate their processes, reducing the time and resources required to perform routine tasks. BPM can also help healthcare organizations identify and eliminate bottlenecks in their processes, allowing them to operate more efficiently and effectively in the long-term. This also saves costs and time. But how do health organizations optimize their digital transformation journey?
Build a Business Case
Stakeholders need to “buy in” to a digital transformation strategy and for that to happen, you need to clearly define your vision and the benefits of automation. Begin with a basic introduction, describing the proposed vision and accompanying benefits. From here, key questions should be addressed: What happens if you do nothing? What are the different possible procurement pathways? Are there multiple deployment options?
It’s important to convey what defines success and how it will be achieved. Longer-term plans should be a part of the equation. How will the proposed solution be procured? Make sure to consider regulations and policies. Information on license costs, projected revenue savings, and proposed returns on investments should be modeled.
While this all may seem daunting to put together, when taken step-by-step and with the advice of experts – it becomes achievable.
Devising and following a strategic plan for digital transformation is the difference between true transformation and short-term wins.
Step 1: Decide What to Automate
This is one of the most important steps. Organizations seem to be best off when they begin with simple, yet high-volume tasks involving multiple people.
By starting with easier wins, you’re able to more easily get people on board through quantifiable proof points of the benefits of digitalization. Cultural adoption is crucial to success, so it’s important to get people involved in goal and roadmap structuring early on. This helps foster an automation-first culture.
Once you’ve identified the opportunities you want to automate, study these processes and consider limitations and workarounds. Understanding processes before automating them is essential. Process intelligence can be especially helpful here since healthcare organizations tend to operate across multiple systems that sit within interoperable siloes. Process mining software can process system-level data to uncover the best tasks to automate, factoring insights and hidden steps that manual assessment can miss. This helps organizations better overcome the inherent limitations of any existing systems.
Step 2: Process Automation Needs Oversight
To successfully deploy process automation, executive sponsorship is important. Transparency across the business is essential to garner the support and credibility needed to onboard the entire organization. This is key because automation success will collapse without the support of entire teams.
Team members should know their roles and responsibilities. They should have a clear understanding of how digital workers will impact them, including direct benefits.
Your developers, engineers, and consultants play an instrumental role in developing and deploying your automation infrastructure. It can be helpful to establish a center of excellence (CoE) to oversee the digital transformation journey, ensuring that actions align with overall strategic objectives and are within regulatory and governance frameworks.
Step 3: Managing the Plan with Opportunities to Scale
At this point, you should have an on-board work environment and the systems needed for success in place. It’s important the establishment of an ongoing operating model, which should include several factors: a long-term strategy that includes scaling plans, clear roles, needed skills – using education and training to fill any gaps, governance measures, and best practices.
Devising and following a strategic plan for digital transformation is the difference between true transformation and short-term wins. Once you have deployed your automations, digital transformation is not complete – it’s an ongoing journey that requires a robust and agile infrastructure, combined with a culture of automation, and leaders to manage the change.
 About Anna Twomey
About Anna Twomey
Anna Twomey is the Senior Director, Healthcare Providers – Americas at SS&C Blue Prism. With more than 25 years of experience as a consultant and advisor in healthcare technology, Anna brings a range of expertise across Disease Surveillance, Accountable Care Organizations (ACO), Population Health Management, Regulatory Compliance, HIPAA Privacy Rule, and the required rulings of CPOE and ARRA. She has led startup, turnaround and high growth initiatives for industry-leading healthcare delivery teams. Equipped with a teaching degree in computer science and multiple post-graduate certifications, she helps healthcare organizations transform healthcare processes and delivery through AI and intelligent automation.
< > Featured Health IT Job: Procurement Coordinator
We like to regularly feature a healthcare IT job that might be of interest to readers. Today, we’re featuring the Procurement Coordinator position that was recently posted on Healthcare IT Central. This position was posted by New York eHealth Collaborative and is a hybrid position requiring one day a week in the Albany, New York office.
Here’s a description of the position:
New York eHealth Collaborative (NYeC) is a not-for-profit organization working in partnership with the New York State Department of Health to improve healthcare by collaboratively leading, connecting, and integrating health information exchange across the State.
Founded in 2006 by healthcare leaders, NYeC works to help New York State achieve the Triple Aim of improving the patient experience of care, delivering better health outcomes, and reducing costs. On behalf of the State, NYeC leads the Statewide Health Information Network for New York (SHIN-NY), a network to connect healthcare providers statewide, develops policies and standards that support the utilization of health technologies, and assists healthcare providers in adopting and effectively using electronic health records.
NYeC is propelling healthcare forward by facilitating the use of new and innovative technologies that will improve patient care. Healthcare is currently undergoing an unprecedented transformation through a digital health revolution do you want to be at the epicenter of it?
Employees must be fully vaccinated in accordance with NYeC’s policy before beginning employment with NYeC and present proof prior to their start date unless they have requested and been granted an exemption or accommodation (based on disability/medical condition or a sincerely held religious belief).
Position Summary
NYeC is seeking a Procurement Coordinator who is a driven and committed team player to assist with the centralized procurement processes. The Procurement Coordinator will report to the Senior Director, SHIN-NY Contract and Project Management. This role will work closely with all teams across the organization and align processes with both the Fiscal and Legal teams.
This role will be based out of our Albany, NY office. At this time, this role has a hybrid work schedule. All staff are required to work in the office 1 day per week (currently Tuesdays). There are then at least 30 additional in-person days that are expected each year on top of the 1 day required per week. Stakeholder visits, all staff meeting days, development days, and conference attendance count towards the additional 30 days. This schedule is subject to change.
Key Responsibilities
- Administer NYeCs centralized procurement processes (i.e. the process for procuring goods and services for the entire organization)
- Assist in the development, review, updating, and implementation of procurement process documents and trainings
- Trainings may include in-person and/or virtual all staff learning sessions
- Administer and maintain NYeCs contract and procurement management system
- Work closely with the program teams to understand the details of the procurement requirements
- Communicate with vendors to request required procurement documents, review submitted documents for completion and compliance with procurement rules and ensure that documents are appropriately routed internally and externally
- Assist with the development and review of all RFPs (Request for Proposals), RFIs (Request for Information), Industry Surveys, scoring instruments, etc.
- Run reports in the contract management program and work with program teams to determine next steps for existing licenses, contracts, etc.
- Create vendor request forms with all supporting documentation for legal review
- Effectively manage and identify solutions to challenges. Identify ways to improve internal work methods, processes, and template documents
- Clearly communicate with others
- Assist the Senior Director, SHIN-NY Contract and Project Management with any vendor or contract performance issues, as requested
- Assist with tracking deliverables, as requested
- Other duties as assigned
Experience and Skills
- High school diploma/GED required
- Associate degree in business administration or a related field preferred
- 2 to 4 years professional working experience in a procurement field
- Good working knowledge of MS Office suite
- Ability to be proactive and take initiative by being a highly-engaged creative thinker and problem solver
- Ability to multi-task, work quickly and accurately, meet deadlines and set priorities
- Exceptional communication skills both verbally and in written form with a variety of stakeholders (including business, policy, technical, legal and operational stakeholders, NYeC leadership, external stakeholders and team members)
- Ability to effectively manage and stick to timelines and update the team if there are any barriers throughout
- Outstanding planning and organizational skills with attention to quality of detail
- Self-starter with strong sense of ownership and involvement
- Occasional travel required (overnight and/or daily, within NY state and to NYeC offices)
- Experience in reviewing and interpretating contract terms and conditions a plus
- Contract management system experience preferred, Agiloft experience a plus
- Experience with Jira, DocuSign and/or Adobe a plus
- Teams video/meeting experience for training staff preferred
We consider a wide range of factors when determining compensation, which may cause compensation to vary depending on your skills, experience, qualifications, and home office location (Manhattan, NY vs. Albany, NY). The annual base salary range for this Albany based role is $60,000 – $65,000. The salary offer will not be based on a candidates salary history at other jobs, and by law, NYeC will not seek information about salary history, and candidates should not share such information with NYeC. All compensation questions and comments should be directed to the HR Department representative during your application, interview, and hiring process.
NYeC is an Equal Opportunity Employer. We are dedicated to building a diverse, inclusive, and authentic workplace, so if you are excited about this role but your past experience doesn’t align perfectly with everything listed in the job description, we encourage you to apply anyways. You may be just the right candidate for this or other roles.
NYeC is an EOE/Minorities/Females/Vet/Disabled.
Looks like a great opportunity for those with experience with coordinating procurements. If this looks like a position that would interest you, check out the full details for the job and how to apply.
As always, you can search our Health IT job board for a variety of jobs from leading companies in the industry. You can also register for free and post your resume where recruiters search for job candidates regularly.
< + > Epic Ambient AI Charting Released and More Updates on Epic’s AI Solutions
Yesterday, Epic held a winter version of their “Cool Stuff Ahead” presentation for their customers that they generally save for their annual...
-
As I’m sure you know, times are tough. Wages have largely remained the same while prices have risen across the board – and healthcare is no ...
-
Solution Erases Long Phone Holds for Patients, Supports Overwhelmed Medical Front Desk Workers, and Improves Patient Access to Physicians A...
-
Announcement written by Zack Kanter, Founder and CEO at Stedi In February of last year, I gathered our engineering team in a war room. Chan...
